TB Treatment: Drugs, Side Effects, and What Actually Works
When it comes to TB treatment, the standardized course of antibiotics used to kill Mycobacterium tuberculosis bacteria. Also known as antitubercular therapy, it’s one of the most time-sensitive and strictly monitored drug regimens in modern medicine. Unlike a simple infection, TB doesn’t go away with a few days of pills. It takes months — often six to nine — and the wrong mix can lead to drug resistance, organ damage, or death.
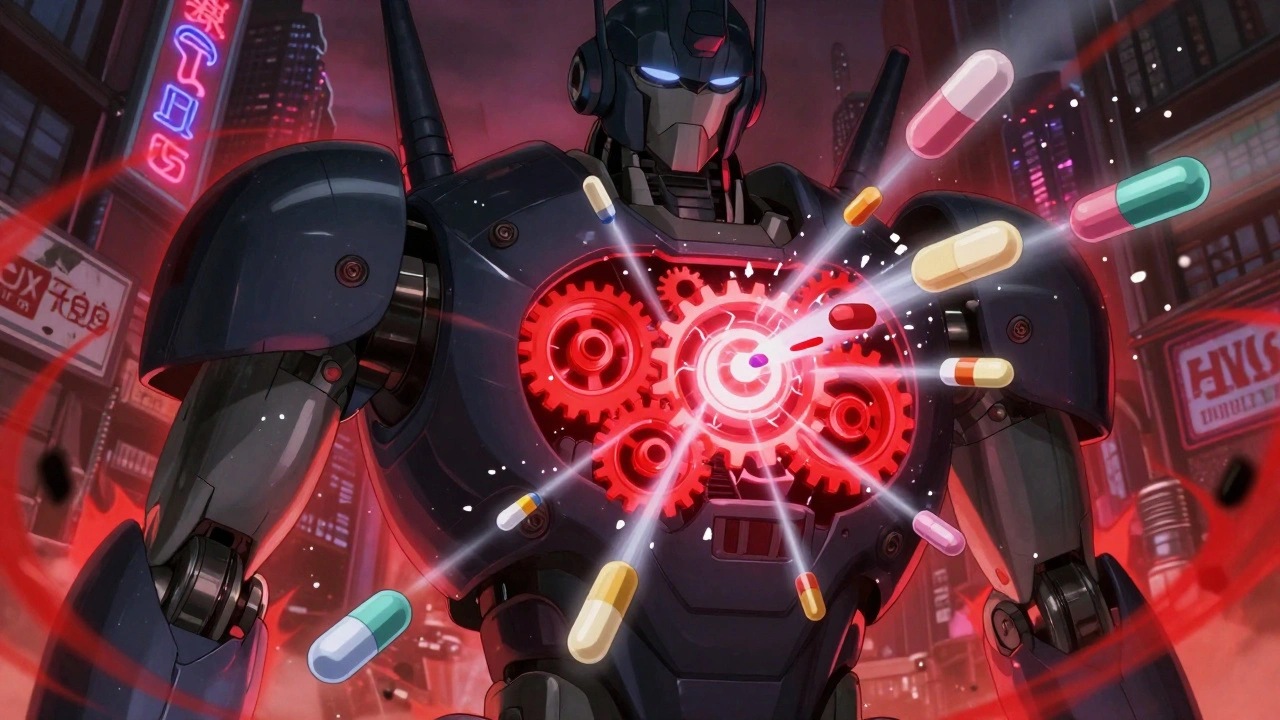
Anti-TB medications, the core drugs used to treat tuberculosis, including isoniazid, rifampin, pyrazinamide, and ethambutol. Also known as first-line TB drugs, they’re taken together from day one to prevent resistance from forming. These aren’t optional. Skipping even a few doses can turn a curable case into a deadly one. And if resistance kicks in, you’re looking at drug-resistant TB, a form of tuberculosis that doesn’t respond to standard first-line drugs, requiring longer, more toxic regimens. Also known as MDR-TB or XDR-TB, it’s harder to treat, costs 100 times more, and has lower survival rates. This isn’t theoretical — the WHO reports over 400,000 new cases of drug-resistant TB every year.
Side effects are common and often misunderstood. Nausea? That’s pyrazinamide. Numb toes or blurry vision? That’s ethambutol. Liver damage? That’s isoniazid. Doctors monitor blood tests every few weeks for a reason. And while some people think herbal remedies or vitamins can replace pills, they can’t. TB bacteria multiply slowly, but they’re relentless. Only proven antibiotics work.
What you won’t hear from every doctor: TB treatment isn’t just about the drugs. It’s about timing, adherence, and support. People who finish their full course are 95% more likely to be cured. Those who stop early? They become the source of new drug-resistant outbreaks. That’s why directly observed therapy — where a nurse watches you swallow each pill — still exists in many countries. It’s not control. It’s survival.
And here’s the hard truth: TB treatment hasn’t changed much in 50 years. We still use the same core drugs. New ones are coming — like bedaquiline and pretomanid — but they’re expensive, hard to access, and reserved for the worst cases. For most people, it’s still isoniazid and rifampin, taken for months, with side effects you can’t ignore.
Below, you’ll find real, practical guides on how these drugs work, what to watch for, how to handle side effects, and why some treatments fail — not because of bad patients, but because of bad systems, poor access, and misinformation. This isn’t theory. It’s what’s happening right now, in clinics and homes around the world. And if you or someone you know is going through TB treatment, you need to know what’s really going on.