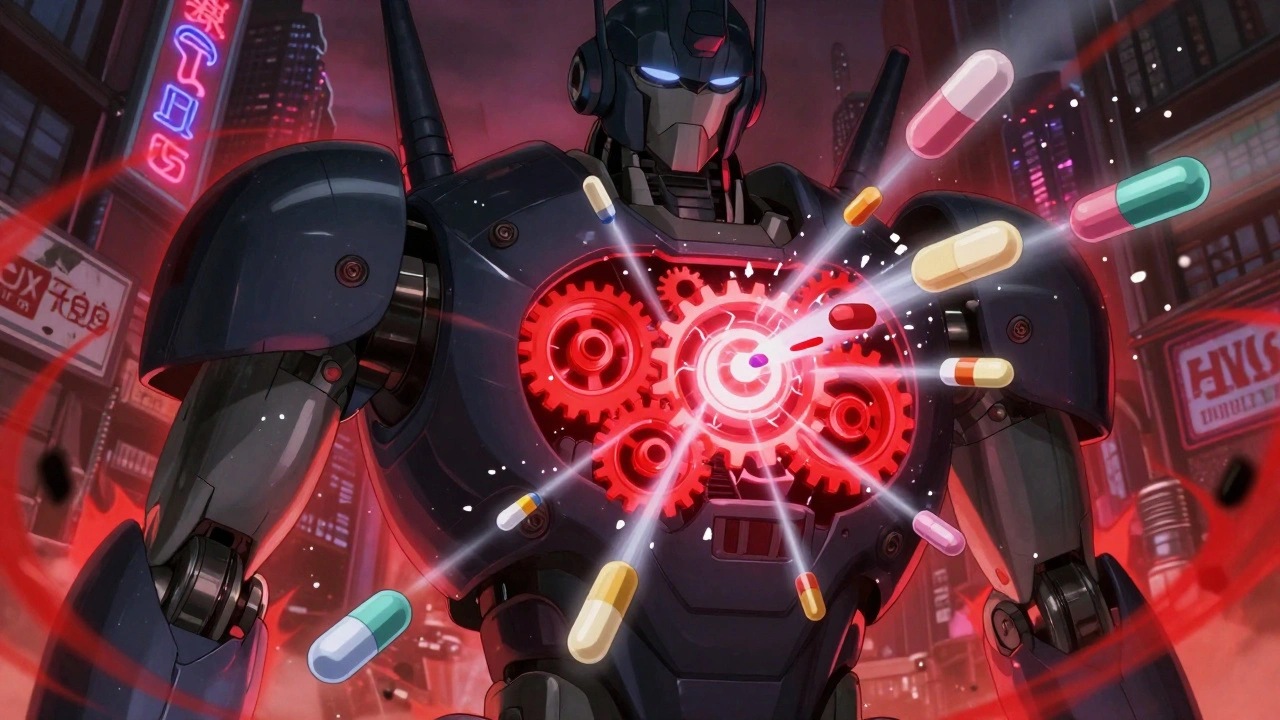
Rifampin Side Effects: What You Need to Know Before Taking It
When you take rifampin, a powerful antibiotic used to treat tuberculosis and prevent meningitis exposure. Also known as Rifadin, it works by stopping bacteria from making RNA, but it doesn’t just target the bad guys—it affects your whole system. Many people notice orange or red urine, tears, or sweat. That’s normal. It’s not a sign something’s wrong; it’s just the drug leaving your body. But if you start feeling dizzy, nauseous, or your skin turns yellow, that’s not normal—and it’s not something to ignore.
Liver damage, a serious risk with rifampin, especially when taken long-term or with other meds. Also known as hepatotoxicity, it can show up as fatigue, dark urine, or pain under your right ribs. Studies show up to 1 in 10 people on rifampin for TB develop abnormal liver tests. It’s rare for it to cause full-blown failure, but if you’re also taking isoniazid, another TB drug that strains the liver. Also known as INH, it can make liver problems worse, your doctor should check your blood every few weeks. Rifampin also speeds up how your body breaks down other drugs—like birth control pills, blood thinners, and even some antidepressants. That means those meds might stop working. If you’re on any regular prescription, tell your doctor you’re starting rifampin. Don’t assume it’s safe just because it’s old or cheap.
Some people get flu-like symptoms, joint pain, or even a sudden drop in platelets. Others report tingling in their hands or feet. These aren’t common, but they happen. And if you’ve had liver disease before, or you drink alcohol regularly, your risk goes up. Rifampin isn’t a drug you take lightly. It’s strong, effective, and necessary for life-threatening infections—but it demands respect. The posts below dig into real cases, how doctors monitor for problems, and what to do if you think something’s off. You’ll find advice on spotting early warning signs, managing interactions, and staying safe while your body fights infection.