Rifampin and CYP3A4: How This Antibiotic Affects Your Other Medications
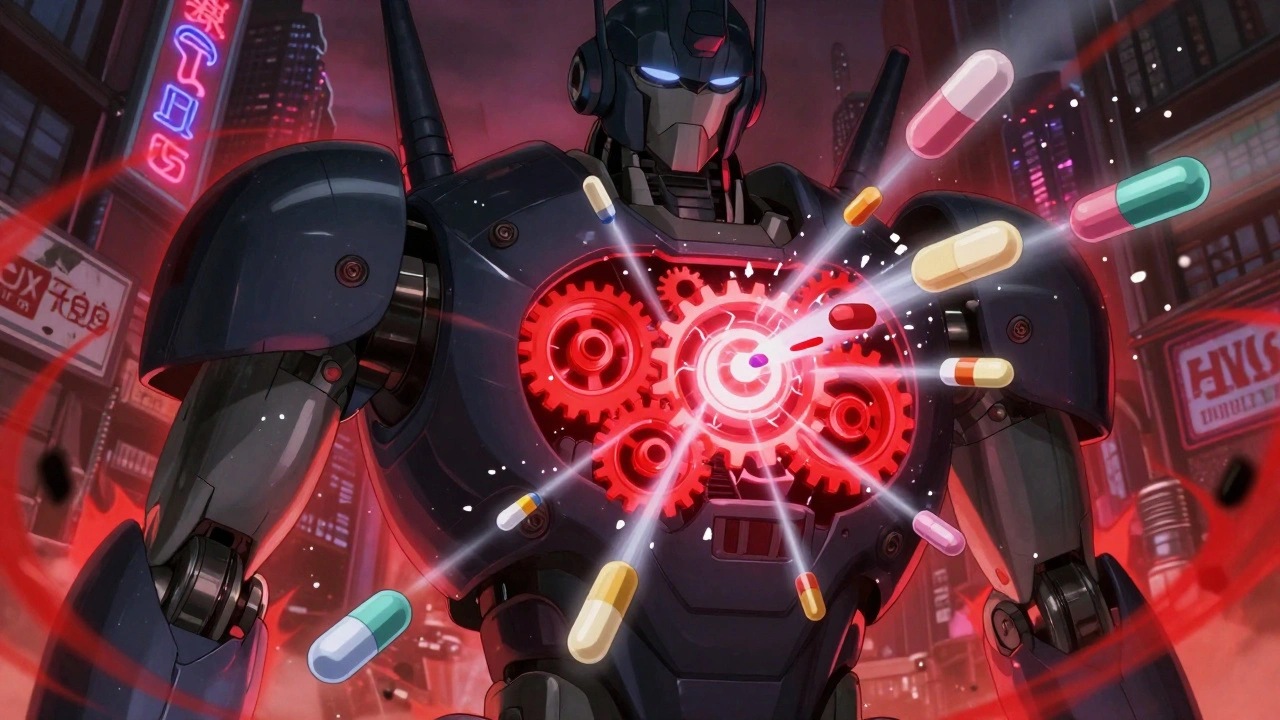
When you take rifampin, a powerful antibiotic used to treat tuberculosis and prevent meningitis exposure. Also known as Rifadin, it doesn’t just kill bacteria—it rewires how your body processes almost everything else you take. This happens because rifampin strongly activates CYP3A4, a key liver enzyme responsible for breaking down over half of all prescription drugs. Think of CYP3A4 as the body’s main drug cleanup crew. Rifampin tells it to work overtime, so other medications get broken down too fast—and stop working.
That’s why people on rifampin often find their birth control fails, their blood thinners lose power, or their HIV meds no longer keep the virus in check. Enzyme induction, the process where drugs like rifampin ramp up enzyme production, isn’t rare—but few are as aggressive as this one. It doesn’t just lower drug levels; it can make life-saving treatments useless. For example, if you’re on an HIV pill like darunavir or a transplant drug like cyclosporine, mixing them with rifampin can lead to treatment failure or organ rejection. Even common drugs like statins, antidepressants, or painkillers can become risky or ineffective. Doctors often have to adjust doses, switch medications, or avoid rifampin entirely if you’re on other critical treatments.
The real danger isn’t just in the interaction—it’s in how invisible it is. You might feel fine, but your drug levels are dropping. That’s why checking for CYP3A4 interactions isn’t optional—it’s essential. This page pulls together real-world cases and clinical insights from posts on drug interactions, medication safety, and how enzymes shape what works in your body. You’ll find guides on how to spot hidden risks, why generics sometimes behave differently under enzyme pressure, and how insurers and pharmacists track these dangerous combos. What you’ll read here isn’t theory—it’s what keeps people out of the hospital.