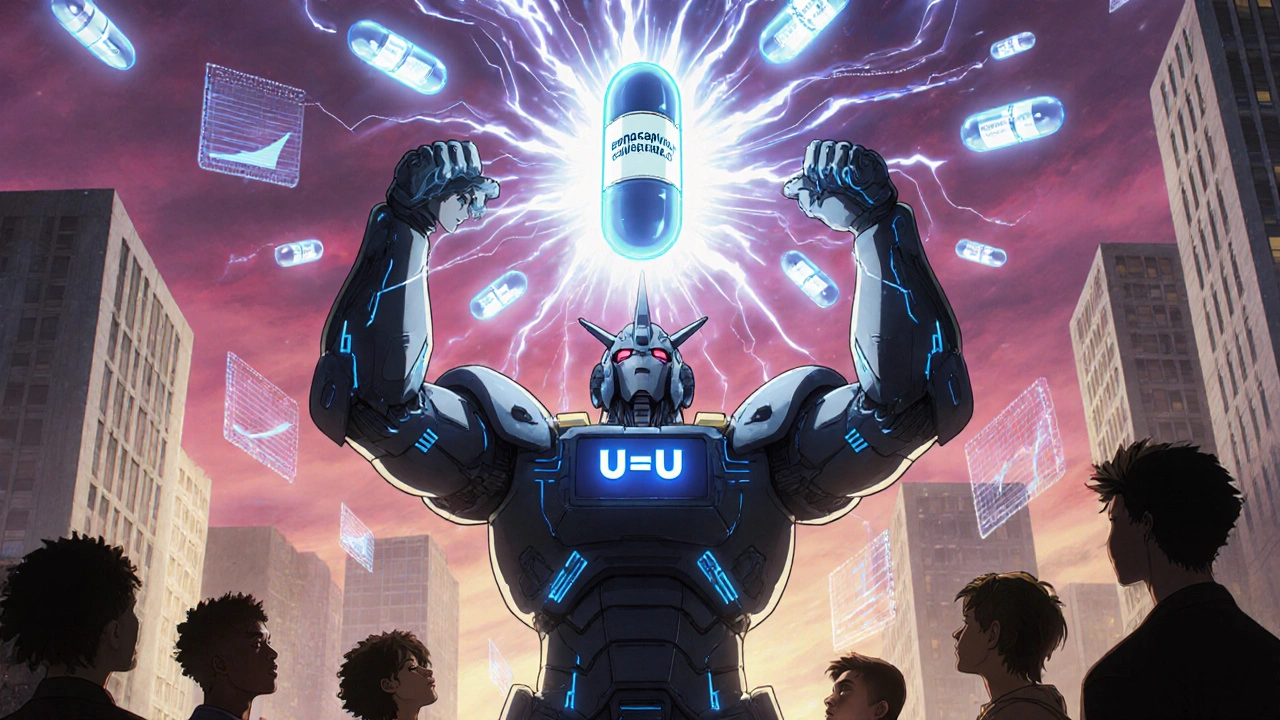
Long-Acting HIV Therapy: What It Is, How It Works, and What You Need to Know
When you hear long-acting HIV therapy, a treatment approach that delivers HIV-fighting drugs through infrequent injections instead of daily pills. Also known as injectable antiretroviral therapy, it’s turning decades of HIV care on its head by cutting daily pill routines down to once a month or even less. This isn’t science fiction—it’s real, FDA-approved, and already helping thousands of people stay undetectable without the stress of remembering a morning pill.
Before long-acting HIV therapy, treatment meant swallowing pills every single day. Miss one, and resistance can creep in. But now, with drugs like cabotegravir and a long-acting integrase inhibitor used in combination with rilpivirine for monthly injections, the game has changed. These drugs stay in your system for weeks, slowly releasing to keep the virus suppressed. They’re not for everyone—your doctor needs to check your viral load first, and you’ll usually start with a short oral lead-in to make sure you tolerate the meds. But for those who struggle with daily adherence, travel often, or just want to reduce pill fatigue, this is a game-changer.
It’s not just about convenience. Studies show people on long-acting HIV therapy are more likely to stick with treatment long-term. That means fewer viral rebounds, less risk of transmission, and better overall health. And while it’s not a cure, it’s the closest thing we have to normalizing life with HIV. The injections are given in the buttocks or thigh, usually by a healthcare provider, and most people report mild soreness—nothing like the nausea or dizziness from some oral meds.
But it’s not all smooth sailing. These therapies require consistent visits to a clinic. If you miss an injection window, your viral load could rise. And they’re expensive—insurance coverage varies widely. Still, the trend is clear: the future of HIV treatment is moving away from pills and toward precision, long-lasting options. As research continues, we’re seeing newer combinations in development, including implants and six-month shots. For now, long-acting HIV therapy is available to adults who’ve already stabilized on oral meds and want a simpler path forward.
What you’ll find in the posts below are real, practical insights from people navigating this shift. You’ll read about how these injections interact with other meds, what side effects to watch for, how they compare to daily pills, and why some patients still prefer the old way. You’ll also see how drug storage, travel, and insurance play into the decision. This isn’t theory—it’s lived experience, backed by clinical data and real-world outcomes. Whether you’re a patient, caregiver, or just trying to understand the latest in HIV care, this collection gives you the facts without the fluff.