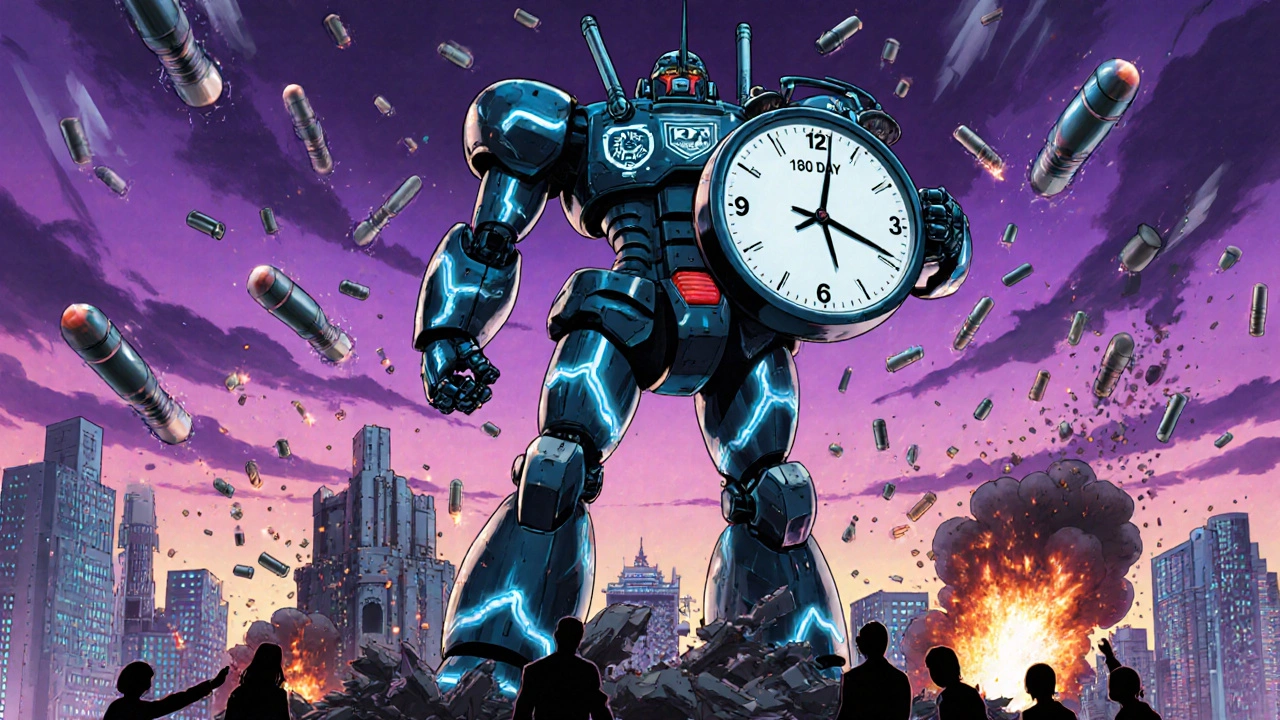
FDA 180-day exclusivity: What it means for generic drugs and your prescription costs
When a brand-name drug’s patent expires, the FDA 180-day exclusivity, a legal incentive given to the first generic manufacturer to challenge a brand drug’s patent and win. Also known as generic market exclusivity, it lets that company be the only generic version sold for six months—before others can enter. This isn’t a reward for innovation. It’s a tool to push down prices fast. The first generic maker gets a head start because they’ve taken the legal risk to break the patent, often spending millions in lawsuits. In return, they get a six-month window where no other generic can compete. That’s when you’ll often see the biggest drop in drug prices.
This system ties directly to how the ANDA, Abbreviated New Drug Application, the filing pathway for generic drugs to prove they’re the same as the brand. Also known as generic drug application, it works. To qualify for the 180-day exclusivity, a company must file an ANDA and successfully challenge a patent. That’s why you’ll see one generic hit the market first, then others follow. But it’s not foolproof. Sometimes, legal delays or multiple challengers mean the exclusivity gets split or lost. And if the first filer doesn’t launch the drug within 75 days after winning, the exclusivity can vanish. That’s why you might wait weeks after a patent expires before a cheap generic appears.
The real impact? Your wallet. During that 180-day window, the first generic is often the cheapest option because it has no competition. After that, more generics flood in—and prices drop even further. But here’s the catch: not every drug gets this treatment. If the patent challenge fails, or if the original maker has multiple patents layered in, the exclusivity might not trigger at all. That’s why some drugs stay expensive for years after patent expiry. The bioequivalence, the scientific proof that a generic delivers the same amount of drug into your bloodstream as the brand. Also known as drug equivalence, it is the foundation of all this. The FDA doesn’t care who files first—they care that the generic works the same. That’s why every generic on your shelf, whether it’s the first or the tenth, has passed the same bioequivalence tests.
What you’ll find in the posts below are real-world examples of how this system plays out. You’ll see how insurers pick which generics to cover, how bioequivalence studies are done, and why some drugs take forever to get cheap. You’ll learn how patent challenges shape what’s on your pharmacy shelf—and why your prescription might cost $2 one month and $20 the next. This isn’t just policy. It’s your medicine. And knowing how it works helps you ask the right questions.