Drug Interactions with Tuberculosis: What You Need to Know
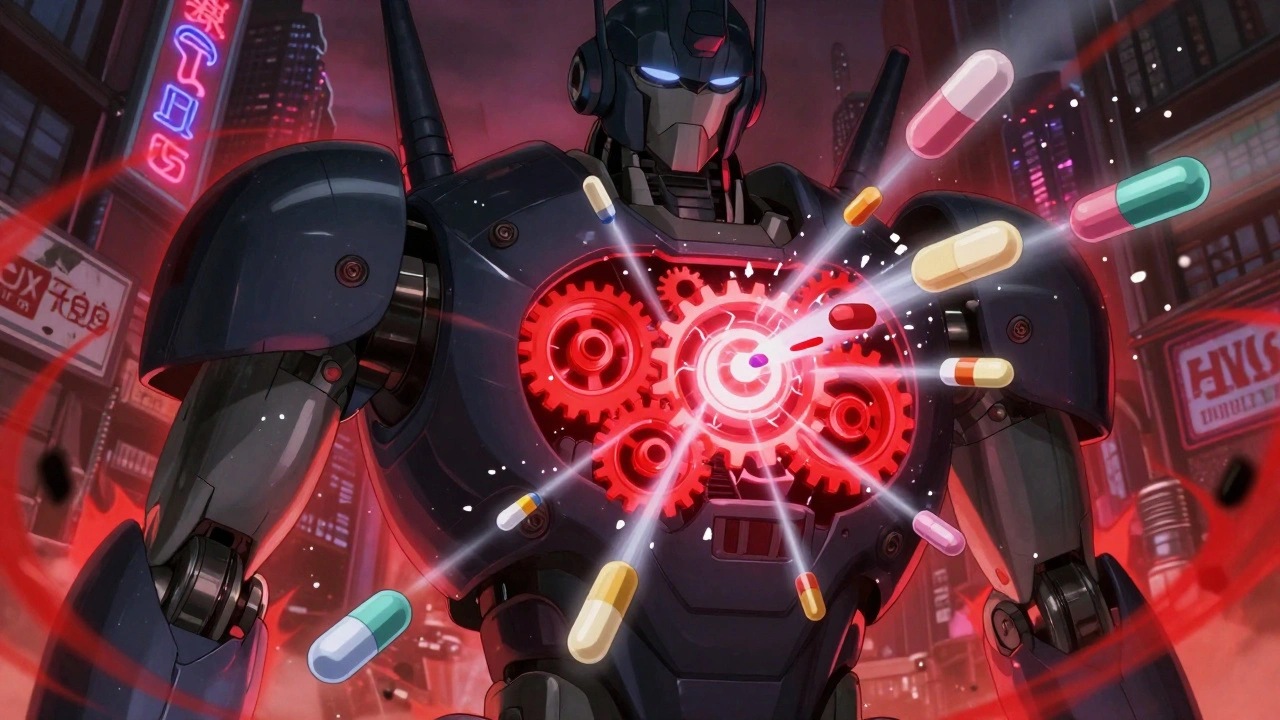
When treating tuberculosis, a bacterial infection that mainly affects the lungs and requires long-term antibiotic therapy. Also known as TB, it's treated with a combo of drugs like rifampin, isoniazid, pyrazinamide, and ethambutol. But these aren't harmless pills—they're powerful medicines that can interfere with everything from birth control to heart meds. Many people don’t realize that taking TB drugs with common medications like statins, antidepressants, or even antacids can lead to serious problems—like liver damage, reduced drug effectiveness, or sudden side effects.
rifampin, a key TB antibiotic that speeds up how your liver breaks down other drugs is the biggest culprit. It can make birth control pills useless, lower the effect of HIV meds like darunavir, and reduce the power of blood thinners like warfarin. If you’re on rifampin and take a daily pill for anxiety or cholesterol, your body might not get enough of it. That’s why doctors check your full med list before starting TB treatment. Another big one is isoniazid, a drug that can cause nerve damage and reacts badly with alcohol or certain seizure meds. Mixing it with alcohol raises your risk of liver failure. Even something as simple as an OTC antacid can mess with how well isoniazid is absorbed.
People with TB often have other health issues—HIV, diabetes, depression—so they’re already on multiple drugs. That’s where things get risky. A study from the CDC found that over 40% of TB patients on rifampin had at least one dangerous interaction with another medication. Some ended up in the hospital because their seizure control failed or their blood sugar spiked. It’s not just about the TB drugs themselves—it’s how they change the way your body handles everything else you take.
What you’ll find below are real, practical guides on how these interactions play out. You’ll see which common drugs clash with TB treatment, how to spot warning signs like yellow skin, strange dizziness, or sudden mood changes, and what to do if you’re already taking something risky. These aren’t theory pieces—they’re based on actual patient cases and clinical data. Whether you’re a patient, caregiver, or just trying to understand why your doctor asked for your whole med list, this collection gives you what you need to stay safe.