
When you’re taking more than one psychiatric medication, the risk of dangerous interactions isn’t just possible-it’s likely. About 30-50% of adverse drug events in psychiatric care come from how these drugs interact with each other, not from the drugs themselves. This isn’t theoretical. People end up in emergency rooms because their antidepressant mixed with an over-the-counter cold medicine triggered serotonin syndrome. Others suffer seizures, heart rhythm problems, or even death from combinations that seemed harmless on paper. The truth is, psychiatric meds don’t work in isolation. They talk to each other-sometimes politely, sometimes violently.
How These Drugs Talk to Each Other
Psychiatric medications don’t just affect your mood. They alter the chemistry of your brain by targeting three key neurotransmitters: serotonin, norepinephrine, and dopamine. Each class of drug has a different fingerprint on these systems. For example, SSRIs like fluoxetine and sertraline boost serotonin. SNRIs like venlafaxine raise both serotonin and norepinephrine. Antipsychotics like risperidone block dopamine. And MAO inhibitors like phenelzine flood the brain with all three. The problem isn’t just what each drug does alone-it’s what happens when they’re stacked. Take fluvoxamine, an SSRI. It doesn’t just increase serotonin. It also shuts down the liver enzyme CYP1A2, which breaks down dozens of other drugs. That means if you’re on fluvoxamine and also take clozapine, the antipsychotic, clozapine builds up in your blood to toxic levels. Same with tramadol, a painkiller. It raises serotonin and blocks reuptake. Combine it with an SSRI, and you’re playing Russian roulette with serotonin syndrome.The Deadliest Combo: MAO Inhibitors and Serotonergic Drugs
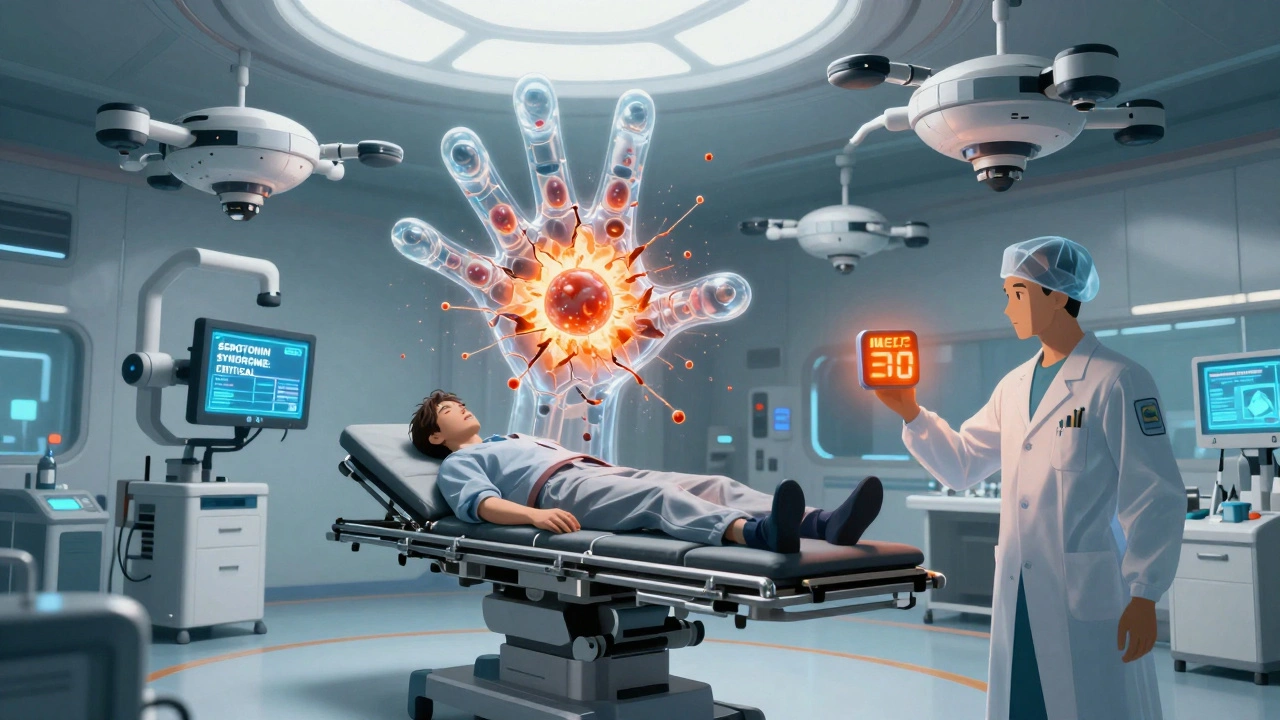
No interaction in psychiatry is more dangerous than mixing MAO inhibitors with any drug that increases serotonin. This includes SSRIs, SNRIs, tricyclic antidepressants, certain opioids like tramadol and meperidine, dextromethorphan (found in cough syrups), and even St. John’s wort. The result? Serotonin syndrome-a condition where your brain gets flooded with too much serotonin. Symptoms start mild: shivering, sweating, restlessness, diarrhea. Then they escalate: high fever, muscle rigidity, seizures, irregular heartbeat. Without quick treatment, death can happen in hours. Mortality rates for severe cases range from 2% to 12%. And here’s the kicker: it can happen within hours of taking the first dose of the second drug. That’s why guidelines demand a two-week washout period between stopping an SSRI and starting an MAOI. No exceptions. No shortcuts. Even some foods matter. MAO inhibitors interact with aged cheeses, cured meats, tap beer, and soy sauce because they contain tyramine. When tyramine isn’t broken down by MAO enzymes, it spikes blood pressure-sometimes to stroke-levels. That’s why patients on phenelzine or tranylcypromine are given strict diet lists. It’s not outdated advice. It’s life-saving.Other High-Risk Combinations You Need to Know
TCAs + Anticholinergics: Tricyclic antidepressants like amitriptyline already cause dry mouth, constipation, blurred vision, and urinary retention. Add antihistamines (like diphenhydramine in Benadryl), antipsychotics, or even some bladder medications, and these side effects multiply. Your heart rate spikes. Your blood pressure drops. You might pass out. In older adults, this combo increases dementia risk and falls. Lithium + NSAIDs: Lithium is one of the most effective mood stabilizers-but it has a razor-thin safety margin. Normal levels are 0.6-1.0 mmol/L. Too high, and you get tremors, confusion, kidney damage, or coma. NSAIDs like ibuprofen or naproxen reduce kidney blood flow, causing lithium to build up. Studies show levels can jump 25-50% after just a few days of NSAID use. That’s why patients on lithium are told to avoid these painkillers unless closely monitored. Quetiapine + CYP3A4 Inhibitors: Quetiapine is broken down by the liver enzyme CYP3A4. If you take it with drugs that block this enzyme-like fluconazole (a yeast infection med), clarithromycin (an antibiotic), or even grapefruit juice-quetiapine levels can double. That means extreme drowsiness, low blood pressure, and risk of sudden cardiac death. The FDA issued a warning about this exact combo in 2020. SSRIs + Warfarin: Warfarin is a blood thinner with a narrow window. Too little, and you clot. Too much, and you bleed. SSRIs like fluoxetine and fluvoxamine interfere with how warfarin is metabolized. INR levels can rise by 20-30% within days. Weekly blood tests are required during the first month of combination therapy.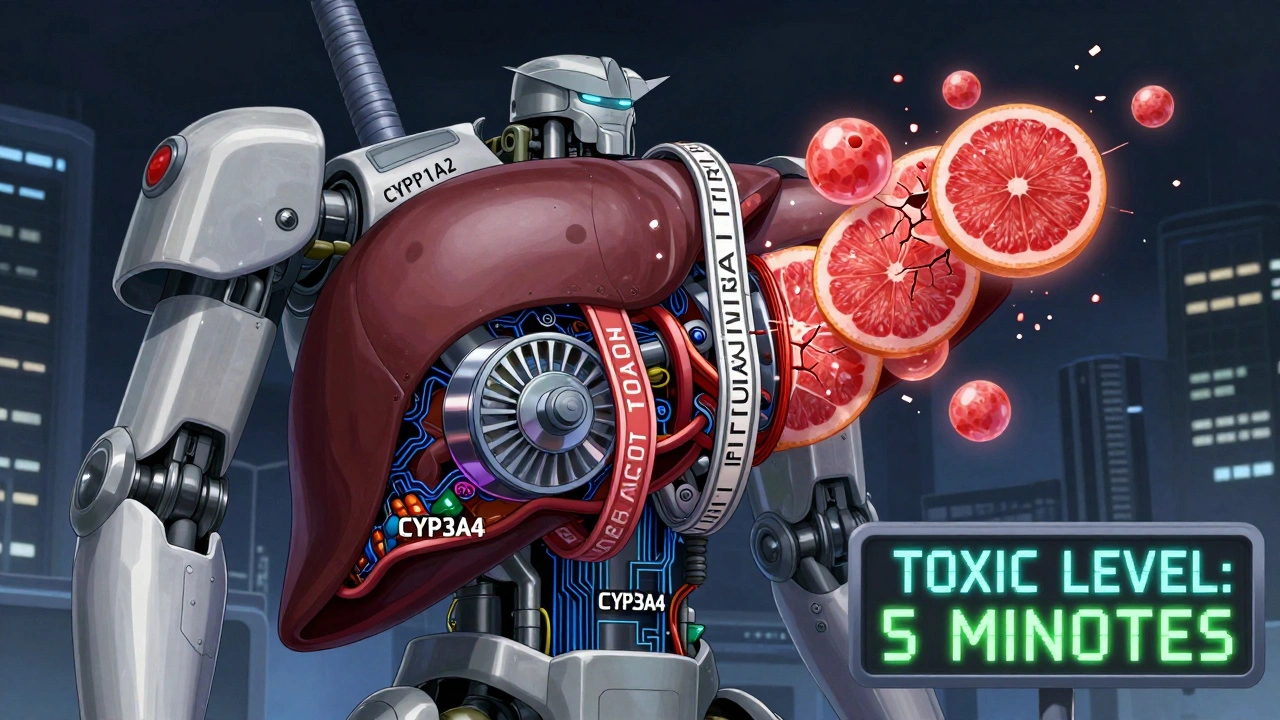
What Makes Some Drugs Safer Than Others
Not all psychiatric drugs are created equal when it comes to interactions. Some are like landmines. Others are low-key. If you’re starting a new medication and already on others, your doctor should pick the safest option first. Sertraline and citalopram are among the safest SSRIs. They don’t strongly block liver enzymes, so they’re less likely to interfere with other meds. Fluoxetine? Not so much. It lingers in your body for weeks and blocks multiple enzymes. That’s why switching from fluoxetine to sertraline is often recommended in complex cases. SNRIs like desvenlafaxine and duloxetine have fewer interactions than TCAs. Atypical antipsychotics vary wildly. Aripiprazole has low interaction risk. Ziprasidone? Higher. Quetiapine? Moderate-but watch the grapefruit juice. Vilazodone and vortioxetine are newer and designed to have minimal enzyme interference. The bottom line: if you’re on three or more psychiatric drugs, your doctor should be asking: “Is this necessary? Is there a safer alternative?” Polypharmacy isn’t always the answer. Sometimes, less is more.How Doctors Monitor for Danger
Good prescribing doesn’t stop at writing a prescription. It includes tracking. The American Association of Psychiatric Pharmacists recommends using standardized tools to catch problems early.- PHQ-9: Monitors depression severity. Scores above 15 mean you need urgent attention.
- GAD-7: Tracks anxiety. Rising scores can signal drug side effects, not worsening illness.
- AIMS: Checks for involuntary movements caused by antipsychotics. Done every 3 months.
- Lithium levels: Tested weekly at first, then monthly. Anything above 1.2 mmol/L is a red flag.
- INR: Checked weekly for the first month if you’re on warfarin and an SSRI.
- Liver enzymes and CBC: Required for clozapine (weekly for 6 months) and valproate (every 3 months).
What You Can Do to Stay Safe
You’re not powerless in this. Here’s what you can do right now:- Keep a complete list of every medication-prescription, OTC, supplements, herbal. Include doses and why you take them.
- Bring this list to every appointment-even if you’ve seen the doctor before.
- Ask: “Could this new med interact with anything I’m already taking?” Don’t assume they know.
- Never start or stop a psychiatric drug without talking to your prescriber. Even a small dose change can trigger an interaction.
- Use a pill organizer with alarms. Missing doses or taking extra pills increases risk.
- Know the signs of serotonin syndrome: agitation, sweating, fever, muscle stiffness, rapid heartbeat. If you feel this, go to the ER immediately.
The Future: Personalized Safety
The field is changing. Pharmacogenomic testing-checking your genes to see how you metabolize drugs-is now available. If you’re a poor metabolizer of CYP2D6 or CYP2C19, certain antidepressants will build up in your body faster. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published clear guidelines for this. Digital tools are helping too. Some EHR systems now flag dangerous combinations in real time. One study showed a 37% drop in serious interactions when these alerts were used properly. The National Institute of Mental Health is testing AI models that predict your personal risk based on your meds, genes, age, and medical history. These won’t replace doctors-but they’ll make them better.Final Reality Check
Psychiatric medications save lives. But they’re not harmless. The more you take, the more you risk. And the more you ignore interactions, the more you gamble with your health. There’s no shame in asking for a simpler regimen. There’s no pride in taking five drugs if three will do. Your brain doesn’t need a chemical storm to feel better. It needs balance. If you’re on multiple psychiatric meds, don’t wait for a crisis. Talk to your doctor. Get a full review. Ask for a medication reconciliation. Your life might depend on it.Can I take over-the-counter cold medicine with my antidepressant?
Many OTC cold medicines contain dextromethorphan or pseudoephedrine, both of which can interact dangerously with antidepressants. Dextromethorphan increases serotonin and can trigger serotonin syndrome when taken with SSRIs or SNRIs. Pseudoephedrine can raise blood pressure, especially if you’re on an MAOI or tricyclic antidepressant. Always check with your pharmacist or doctor before taking any OTC product.
How long should I wait between stopping an SSRI and starting an MAOI?
You must wait at least two weeks after stopping an SSRI before starting an MAOI. For fluoxetine, which stays in your system longer, wait five weeks. This washout period prevents serotonin buildup that can lead to serotonin syndrome. Never shorten this time-even if you feel fine.
Is it safe to drink alcohol while on psychiatric meds?
Alcohol is risky with almost all psychiatric medications. With SSRIs, it can worsen depression and increase drowsiness. With benzodiazepines or antipsychotics, it can cause dangerous sedation and breathing problems. With TCAs or MAOIs, it raises the risk of sudden drops in blood pressure and liver damage. Most experts recommend avoiding alcohol entirely while on these drugs.
What should I do if I miss a dose of my psychiatric medication?
Don’t double up. Missing one dose usually won’t cause harm, but taking extra can trigger side effects or interactions. If you miss a dose, take it as soon as you remember-unless it’s close to your next dose. Then skip it. Consistency matters more than perfection. Talk to your doctor if you’re missing doses often.
Can herbal supplements like St. John’s wort interact with antidepressants?
Yes. St. John’s wort is a potent serotonin enhancer and can cause serotonin syndrome when combined with SSRIs, SNRIs, or MAOIs. It also interferes with the metabolism of many drugs, including birth control, blood thinners, and HIV meds. Many people assume natural means safe-but that’s not true. Always tell your doctor about every supplement you take.
Are there any psychiatric drugs that are safer to combine?
Yes. Some drugs have lower interaction risks. Sertraline, citalopram, and escitalopram (SSRIs) are generally safer than fluoxetine. Desvenlafaxine and duloxetine (SNRIs) have fewer enzyme interactions than TCAs. Aripiprazole and lurasidone (antipsychotics) have lower interaction potential than quetiapine or risperidone. When possible, doctors choose these agents for patients on multiple medications.

Joe Lam
December 4, 2025 AT 01:12This post reads like a pharmaceutical industry pamphlet dressed up as medical advice. Everyone knows SSRIs are overprescribed like candy, but nobody wants to admit the system’s broken. You’re telling me we need a 2-week washout period but doctors are still stacking meds like Jenga blocks? Wake up. The real danger isn’t the drugs-it’s the profit-driven, checklist psychiatry that treats brains like malfunctioning circuit boards.
jagdish kumar
December 4, 2025 AT 22:44Chemical balance is a myth. The mind is not a beaker. You pour serotonin in, you pour dopamine out… and call it treatment? The body remembers what the mind forgets. These drugs are not fixes-they are temporary silencers of a soul screaming for meaning.
zac grant
December 6, 2025 AT 06:09Great breakdown-especially the CYP enzyme stuff. Clinically, this is gold. For anyone on polypharmacy, the key is metabolic profiling. If you’re a CYP2D6 poor metabolizer, fluoxetine is a ticking bomb. Sertraline? Much safer. Also, always check for CYP3A4 inhibitors if you’re on quetiapine. Grapefruit juice isn’t just for breakfast anymore-it’s a cardiac risk factor. And yes, AIMS scoring every 3 months? Non-negotiable. Document everything. Your pharmacist can be your best ally here.
Pavan Kankala
December 6, 2025 AT 20:15They want you to believe this is science. But who funds the studies? Pharma. Who writes the guidelines? Pharma. Who gets paid when you’re on five meds? Pharma. The whole ‘serotonin syndrome’ scare? A way to scare you into compliance. They want you dependent. The real cure? Fasting, sunlight, and quitting social media. But they won’t tell you that because it doesn’t come in a pill bottle.
Jessica Baydowicz
December 7, 2025 AT 08:38OMG this is SO important!! I was on Lexapro + DayQuil and had this weird buzzing feeling like my nerves were dancing 😅 I thought I was losing it-turns out it was serotonin stuff!! Now I keep a meds list on my phone and show it to every doc. Also, St. John’s Wort? Nope. Not even ‘natural’ vibes. Your brain deserves better than a chemical cocktail. You got this!! 💪❤️
John Filby
December 8, 2025 AT 06:00Just wanted to say thanks for this. I’m on 4 meds and was terrified to ask my doc if any were clashing. Now I’m bringing this list to my next appointment. Also, the pill organizer tip? Genius. I started using one with alarms and haven’t missed a dose in 3 weeks. Small wins, ya know? 🙌
Elizabeth Crutchfield
December 9, 2025 AT 21:20i read this and just cried. my mom died from a bad combo. she took her abilify and some advil for her back and the lithium kicked in too hard… no one told her. please, please, please talk to your dr. and your pharmacist. i’m still mad but i’m also trying to help others. you’re not alone.
Rachel Bonaparte
December 9, 2025 AT 21:45Let’s be real-this is all just a distraction. The real issue isn’t drug interactions, it’s the fact that our entire mental health infrastructure is a corporate Ponzi scheme. They don’t want you healed. They want you medicated. The two-week washout? A loophole they invented to keep you hooked. The FDA? Bought and paid for. The AI models they’re testing? Just a fancy way to collect your genetic data for insurance discrimination later. And don’t get me started on pharmacogenomics-your DNA isn’t the problem. The system is. They’re turning your brain into a commodity. You’re not a patient-you’re a revenue stream. Wake up before your next blood test becomes your obituary.
Scott van Haastrecht
December 11, 2025 AT 19:19So let me get this straight-you wrote a 2,000-word essay on drug interactions and didn’t once mention that psychiatrists are the #1 prescribers of opioids in the US? That’s the real crisis. You’re scared of serotonin syndrome? Try living with the 40% of patients who get prescribed antipsychotics for insomnia. Or the 12-year-old on five meds because their teacher said they were ‘disruptive.’ This isn’t medicine. It’s chemical containment. And you’re just the PR guy for the prison.