
Proton pump inhibitors, or PPIs, are among the most common medications people take for heartburn, acid reflux, and stomach ulcers. Brands like Prilosec, Nexium, and Protonix are everywhere - on pharmacy shelves, in medicine cabinets, and in daily routines. Many people take them without thinking twice, assuming they’re harmless because they’re available over the counter. But what if taking them for months or years is doing more harm than good?
How PPIs Work - And Why They’re So Popular
PPIs work by shutting down the acid-producing pumps in your stomach lining. These pumps, called H+/K+ ATPase, are the final step in making stomach acid. By blocking them, PPIs cut acid production by up to 95%. That’s why they’re so effective. If you have erosive esophagitis, PPIs heal it in over 90% of cases. They’re the gold standard.
But here’s the catch: they’re not meant to be taken forever. Most guidelines say 4 to 8 weeks for uncomplicated heartburn. Yet, studies show that up to 70% of people taking PPIs don’t even need them. Many are using them because their doctor prescribed them years ago and never checked back. Or they bought them over the counter and just kept going.
The Hidden Risks of Long-Term Use
When you take PPIs for more than a year, your body starts to react in ways you might not expect. The FDA has issued multiple safety alerts since 2010, and here’s what the evidence shows:
- Low magnesium (hypomagnesemia): This is rare, but serious. Symptoms include muscle cramps, irregular heartbeat, and seizures. The FDA now says doctors should check magnesium levels in anyone on PPIs for over a year.
- Increased risk of bone fractures: Especially hip fractures. A 2017 study found people who took PPIs for 6 to 8 years had a 55% higher risk. The good news? That risk drops back to normal within two years of stopping.
- Vitamin B12 deficiency: PPIs reduce stomach acid, which your body needs to pull B12 out of food. About 10-15% of long-term users become deficient. That can lead to fatigue, nerve damage, and brain fog.
- C. diff infection: Your stomach acid normally kills harmful bacteria. With less acid, C. difficile can survive and cause severe diarrhea. Hospitalized patients on PPIs have nearly double the risk.
- Acute interstitial nephritis: A rare but serious kidney inflammation. It’s often reversible if caught early, but can lead to chronic kidney disease if ignored.
Some studies have linked PPIs to dementia, heart disease, and kidney failure. But here’s the truth: those studies mostly looked at people who were already sick - older, sicker, taking multiple meds. It’s hard to say if PPIs caused those problems, or if they were just a side effect of other health issues.
One 2023 study claimed a 44% higher dementia risk in PPI users. But follow-up research showed no link when they controlled for age, diabetes, and other conditions. So while it’s worth being aware of, don’t panic.
Rebound Acid - The Big Reason People Can’t Quit
If you’ve ever tried to stop PPIs and felt worse than before, you’re not alone. About 40 to 80% of people who stop suddenly experience rebound acid hypersecretion. Your stomach, used to being quiet, goes into overdrive. Heartburn returns - often worse than before.
This isn’t addiction. It’s physiology. Your body compensates for the lack of acid by making more of the enzymes that produce it. When you stop the drug, those enzymes go unchecked.
That’s why quitting cold turkey doesn’t work. You need a plan.
How to Stop PPIs Safely
Stopping PPIs isn’t about willpower. It’s about strategy. Here’s what actually works:
- Reduce your dose by half. If you’re taking 40mg daily, go to 20mg. Stay there for 1-2 weeks.
- Switch to every-other-day dosing. After another week or two, cut frequency. Take it only on days you feel symptoms.
- Use H2 blockers as needed. Medications like famotidine (Pepcid) or ranitidine (if available) can help manage rebound acid. They’re not as strong as PPIs, but they’re safer for short-term use.
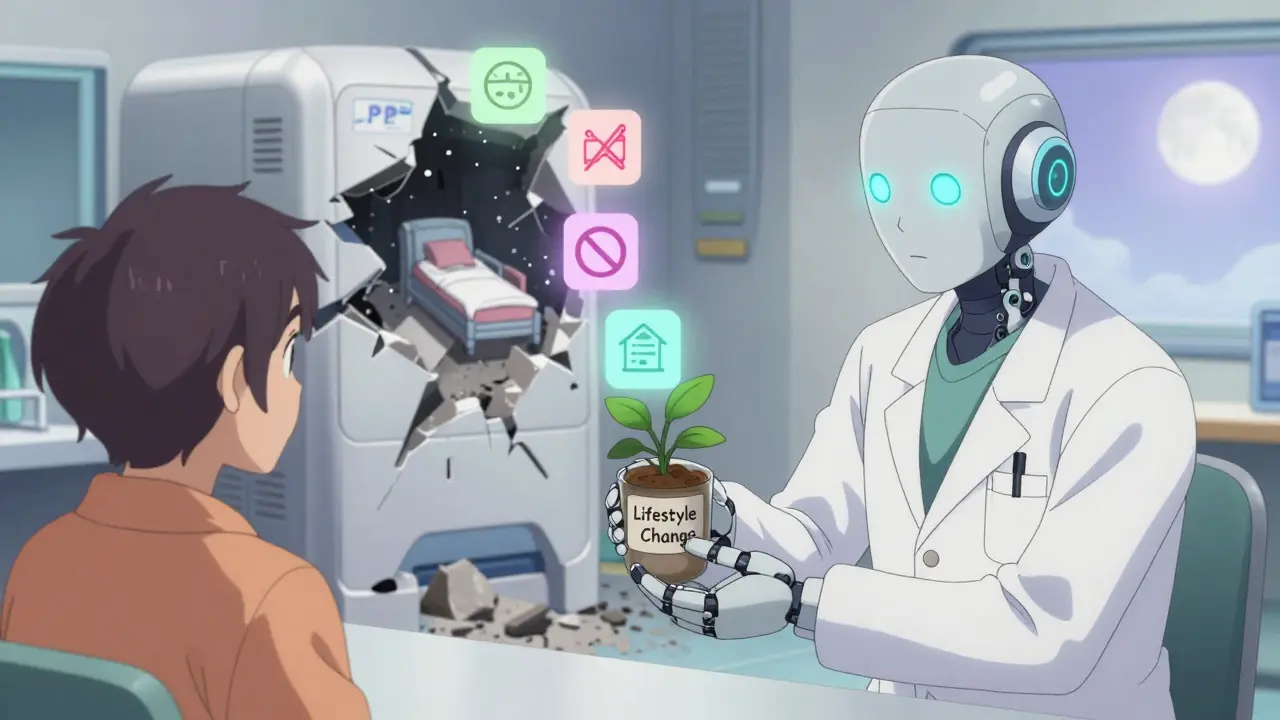
- Try lifestyle changes. Elevate your head while sleeping. Avoid late-night meals. Cut out alcohol, caffeine, spicy food, and chocolate. Lose weight if you’re overweight. These aren’t just “nice to have” - they’re proven to reduce reflux.
- Give it time. Rebound symptoms usually peak around week 2 and fade by week 4. Most people feel normal again within 6-8 weeks.
Some people need help from their doctor. If you’ve been on PPIs for more than a year, ask about a “drug holiday” - a supervised trial of stopping or reducing the dose. Studies show 30-50% of long-term users can stop without symptoms returning, if they do it right.
When You Should Keep Taking PPIs
Not everyone should stop. If you have:
- Severe esophagitis (damaged esophagus from acid)
- Barrett’s esophagus (a precancerous condition)
- History of bleeding ulcers
- Chronic use of NSAIDs like ibuprofen or aspirin
Then PPIs are still the right choice. The risks of stopping outweigh the risks of continuing. But even then, you should be on the lowest dose possible - and get checked yearly.
Over-the-Counter PPIs - A Dangerous Habit
The FDA says OTC PPIs should only be used for 14 days, no more than once every 3 months. Yet, 25% of people using them keep going beyond that. Why? Because they feel better - temporarily. But they’re masking symptoms, not fixing the cause.
Many people use OTC PPIs for bloating, indigestion, or “feeling full too fast.” But those aren’t signs of acid reflux. They could be signs of gallbladder trouble, stomach cancer, or other issues. Self-treating with PPIs delays diagnosis.
If you’re buying PPIs over the counter every few months, it’s time to talk to a doctor. Not a pharmacist. Not Google. A doctor.
What’s Next? New Drugs on the Horizon
There’s new hope on the horizon. A class of drugs called potassium-competitive acid blockers (P-CABs), like vonoprazan, are being studied. They work faster than PPIs, last longer, and may not cause the same rebound effect. But they’re not yet approved in the U.S., and long-term safety data is still limited.
For now, PPIs are still the best tool we have for serious acid-related diseases. But they’re not a lifestyle medication. They’re a medical treatment - and like all treatments, they need monitoring.
Bottom Line: Don’t Fear PPIs. Respect Them.
PPIs saved lives. They healed ulcers, prevented bleeding, and gave millions relief from pain. But they’re not candy. They’re powerful drugs with real, documented risks when used too long.
If you’ve been on a PPI for more than 6 months - especially if you’re taking it daily - it’s time to have a conversation with your doctor. Ask: Why am I still on this? Is there another way? Can I try to stop?
You don’t have to suffer. But you also don’t have to keep taking a drug just because you started it years ago. With the right plan, most people can get off PPIs safely - and feel better than ever.
Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly often causes severe rebound acid reflux, making symptoms worse than before. This happens in 40-80% of people who’ve used PPIs for more than a few months. Instead, taper the dose slowly over weeks - reduce by half, then switch to every-other-day use, and use H2 blockers like Pepcid as needed. Give your body time to readjust.
Are PPIs linked to kidney disease?
There’s a link to acute interstitial nephritis - a rare but serious kidney inflammation - especially after long-term use. The FDA confirmed this in 2016. However, the risk of progressing to chronic kidney disease is still debated. Most cases of kidney injury from PPIs are reversible if caught early. Regular check-ups and monitoring kidney function are important if you’re on PPIs for over a year.
Do PPIs cause vitamin B12 deficiency?
Yes. Long-term PPI use - especially over two years - can reduce your body’s ability to absorb vitamin B12 from food. About 10-15% of users become deficient. Symptoms include fatigue, tingling in hands and feet, memory problems, and balance issues. If you’ve been on PPIs for a long time, ask your doctor for a blood test. Supplementation may be needed.
Can I use antacids instead of PPIs?
Antacids like Tums or Rolaids work fast but only last a few hours. They’re great for occasional heartburn but not for ongoing reflux or esophagitis. PPIs are much stronger and heal damaged tissue. If you have mild, infrequent symptoms, antacids or H2 blockers like Pepcid are safer long-term options. But if you have serious reflux, PPIs are still the most effective treatment - just use them as directed and reassess regularly.
How do I know if I really need a PPI?
You need a PPI if you have confirmed acid-related damage - like esophagitis, Barrett’s esophagus, or a history of bleeding ulcers. If you’re using it for occasional heartburn, bloating, or indigestion without a diagnosis, you likely don’t need it. Ask your doctor: “Was this prescribed for a specific condition? Has it been re-evaluated in the last year?” If not, it’s time to reconsider.
Are over-the-counter PPIs safer than prescription ones?
No. OTC and prescription PPIs are the same drugs, just in different doses. The FDA limits OTC use to 14 days every 3 months because long-term self-medication increases risk. Many people ignore this and use them daily. That’s dangerous. Whether it’s bought at a pharmacy or prescribed by a doctor, PPIs carry the same risks with prolonged use.
What are the alternatives to PPIs?
For mild symptoms, try H2 blockers (famotidine, ranitidine), lifestyle changes (weight loss, no late meals, avoiding trigger foods), and elevating your head while sleeping. For moderate to severe cases, endoscopic treatments like the LINX device or fundoplication surgery may be options. New drugs called P-CABs (like vonoprazan) are promising but not yet widely available. Always discuss alternatives with your doctor - don’t switch on your own.
Next Steps: What to Do Today
- If you’re on a PPI daily and it’s been more than a year - write down why you started it. Did your doctor review it since?
- If you’re taking OTC PPIs more than 14 days at a time - stop. Talk to your doctor instead.
- If you’re feeling better - ask if you can try reducing the dose. Don’t assume you need it forever.
- Keep a symptom journal for two weeks. Note when heartburn happens. Is it after meals? At night? After stress? This helps your doctor decide if you still need the drug.
PPIs are powerful tools. But like any tool, they’re only safe when used the right way. Don’t let convenience turn into risk. Your stomach isn’t the only thing that needs care - your long-term health does too.

Dana Termini
January 7, 2026 AT 09:36I’ve been on PPIs for 5 years because my doctor said it was fine. This post made me realize I never actually got re-evaluated. I’m scheduling an appointment next week to talk about tapering off.
Isaac Jules
January 8, 2026 AT 23:51Wow. Another fear-mongering article disguised as ‘medical advice.’ People stop PPIs cold turkey and then blame the drug when they get worse heartburn. That’s not science, that’s ignorance. The real issue? People want magic pills and refuse to change their diet. Eat less junk, stop lying down after meals, and maybe you won’t need a pill at all. But nope - let’s blame Big Pharma.
Amy Le
January 9, 2026 AT 22:45Let’s be real: PPIs are the pharmaceutical industry’s cash cow. 🤑 They’re not ‘necessary’ for 90% of users. I’ve seen patients on Nexium for 12 years who never had an ulcer - just ‘a little indigestion.’ And now? They’re on magnesium supplements, B12 shots, and kidney monitors. This isn’t medicine. It’s corporate inertia. Doctors prescribe because it’s easy. Patients take because it ‘works.’ No one asks: ‘Why?’
And don’t get me started on OTC PPIs. You can buy them next to gum and candy. That’s not healthcare - that’s a public health disaster waiting to happen. The FDA’s warnings? Too little, too late.
Meanwhile, the real solution? Lifestyle. Sleep elevation. Weight loss. Stress management. But those don’t come in a bottle. So we keep popping pills. And pretending we’re being proactive.
It’s not about fear. It’s about accountability. And nobody wants to be accountable.
Pavan Vora
January 11, 2026 AT 08:01From India, we don't have PPIs everywhere like USA... but when people take it, they take it forever. My uncle took omeprazole for 8 years for 'gas'... then got kidney issue... now he is on dialysis. No one checked him. No one asked why. Just... pills. I think this is global problem. Not just USA. Doctors are busy. Patients are lazy. Pills are cheap. Result? Disaster.
Lily Lilyy
January 13, 2026 AT 07:21This is such an important topic! So many people don’t realize how powerful these medications are. I’m so glad someone is talking about this. If you’ve been on PPIs for a while, please talk to your doctor - you don’t have to live with side effects. There’s hope, and you’re not alone. 💪
Susan Arlene
January 13, 2026 AT 13:45Been on prilosec since 2018. Tried to quit once. Felt like my throat was on fire for two weeks. Ended up back on it. I’m not even sure why anymore. Just…习惯了. Guess I’m gonna try the taper thing now.
Katelyn Slack
January 15, 2026 AT 04:21I’ve been off PPIs for 8 months now. Took 3 months to taper. Used Pepcid when I needed it. Cut out coffee after 4pm. Lost 15 lbs. No more burning. My doctor was skeptical. But it worked. You can do it.
Melanie Clark
January 17, 2026 AT 02:17They’re hiding the truth. PPIs cause cancer. They cause dementia. They cause infertility. The FDA knows. The doctors know. But they’re too scared to say it. You think this is about acid? No. It’s about control. They want you dependent. You think you’re healing? You’re being chemically tamed. Wake up.
Venkataramanan Viswanathan
January 18, 2026 AT 21:06As an Indian doctor, I see this every day. Patients come in saying, 'Doctor, I take PPI every day for bloating.' I ask, 'When did you start?' They say, 'Two years ago.' I ask, 'Did you get an endoscopy?' They say, 'No.' I ask, 'Did you change your diet?' They say, 'No.' Then I say, 'Stop the pill. Try yoga. Eat early. Walk after meals.' Most improve. But they still want the pill. Because change is hard.
Wesley Pereira
January 20, 2026 AT 03:43So let me get this straight - you’re telling me the only reason people are on PPIs is because they’re too lazy to eat a salad? 😏 I’ve got a patient who’s on 40mg daily because she ‘eats pizza on Sundays.’ Bro. That’s not a medical condition. That’s a lifestyle choice. And now she’s got low magnesium and a B12 deficiency. Congrats. You turned a 14-day fix into a lifelong dependency. Well done.
Joann Absi
January 21, 2026 AT 08:00OMG I just realized I’ve been buying OTC PPIs every 2 months since 2020. I thought I was being smart. Now I’m crying. 😭 I’ve been ‘indigestion’ for 5 years but never had an endoscopy. What if I have cancer?? I’m going to the doctor tomorrow. Please pray for me.
Mukesh Pareek
January 22, 2026 AT 22:39Rebound acid hypersecretion is a well-documented pharmacological phenomenon, not a myth. The upregulation of H+/K+ ATPase expression and parietal cell hypertrophy are direct consequences of prolonged proton pump inhibition. This is basic GI pharmacology. The notion that patients are ‘addicted’ is inaccurate - it is physiological adaptation. Management requires stepwise withdrawal, not abrupt cessation.
Ashley S
January 23, 2026 AT 13:57Everyone’s so obsessed with PPIs. What about all the people who just have a sensitive stomach? Maybe you’re just eating too much processed food. Maybe you’re stressed. Maybe you’re drinking too much soda. Why is everything a pill? Why can’t we just… eat better? Stop blaming the drug. Start blaming your habits.
Jeane Hendrix
January 23, 2026 AT 21:14My doctor told me to try the tapering plan. I did it over 6 weeks. Used Pepcid at night. Cut out chocolate and wine. And honestly? I feel better than I have in years. No more brain fog. My energy came back. I didn’t even realize how bad the B12 deficiency was until I stopped. This isn’t just about acid - it’s about your whole body. Thank you for this.