Switching from a brand-name drug to a generic feels like a simple cost-saving move-until you start feeling like it’s not working. You’re not imagining it. The difference isn’t in the chemistry. It’s in your brain.
Why Your Brain Believes the Expensive Pill Works Better
You take a pill. It’s the same active ingredient, same dosage, same manufacturer, same FDA approval. But one bottle says "Lipitor," the other says "atorvastatin." One costs $4.83 a pill. The other, 8 cents. If you didn’t know which was which, you’d feel the same relief. But you do know. And that changes everything.That’s the placebo effect in action-except it’s not about fake pills. It’s about real pills with fake expectations. In a 2014 study, people given sugar pills labeled as a brand-name painkiller reported the same headache relief as those taking actual ibuprofen. The same sugar pills labeled as generic? Half the effect. The brain doesn’t just respond to chemicals. It responds to belief.
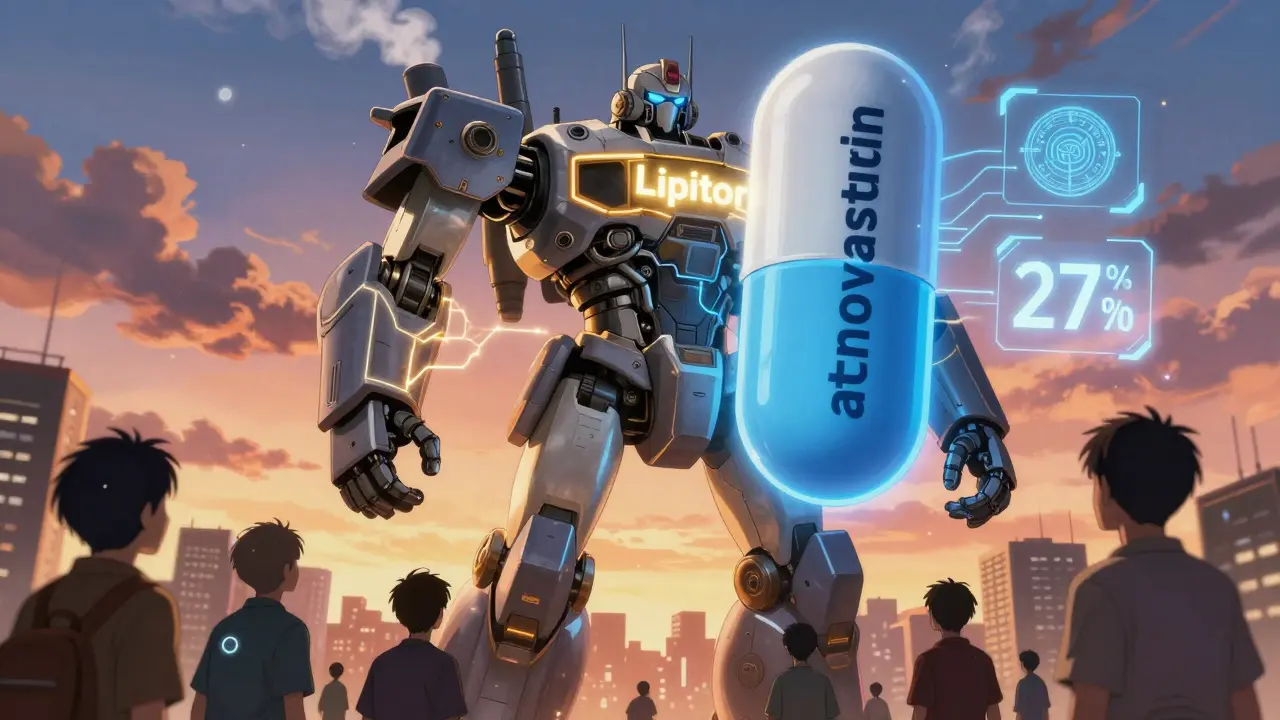
Brain scans show why. When people think they’re taking a brand-name drug, the dorsolateral prefrontal cortex-the area tied to expectation and reward-lights up 27% more than when they think they’re taking a generic. That neural activity isn’t just symbolic. It triggers real pain-relieving chemicals in the body. Your mind isn’t tricking you. It’s healing you.
The Cost-Per-Pill Illusion
It’s not just the name on the bottle. It’s the price tag. In one experiment, healthy volunteers received identical electric shocks and were given placebo pills labeled either $2.50 or $0.10. Those who thought they took the expensive pill reported 64% less pain. The cheaper one? Barely any effect.This isn’t about being gullible. It’s about a lifetime of conditioning. We’re told expensive things are better. Luxury cars, designer clothes, premium coffee. So when your doctor says, "This generic version is just as good," your brain says, "Prove it." And if you’ve been on brand-name medication for years, your body has learned to expect a certain level of relief. Switching to a cheaper version? Your nervous system doesn’t get the signal.
That’s why, in real-world studies, people on generic statins report muscle pain at nearly twice the rate of those on brand-name statins-even when they’re taking a placebo. The difference? Knowing it’s generic. That’s not side effects. That’s a nocebo effect: negative expectations causing real symptoms.
Generics Work-But Only If You Believe They Do
The science is clear: generics are bioequivalent. The FDA requires them to deliver 80-125% of the same blood concentration as the brand. That’s not a loophole. That’s a tight, scientifically validated standard. A 2016 analysis of over 1,000 studies found no meaningful difference in effectiveness between generics and brands across 12 major drug classes.So why do 30% of patients still think generics don’t work? Because perception doesn’t follow data. On Drugs.com, 78% of users who switched from brand to generic reported reduced effectiveness. One person wrote: "My blood pressure jumped 15 points after switching to generic levothyroxine." But lab tests showed identical thyroid hormone levels. The body didn’t change. The belief did.
This hits hardest with chronic conditions. For heart disease, depression, or thyroid disorders, adherence matters more than the pill’s label. A 2016 study found brand-name users were 18% more likely to keep taking their medication after a year-even when the generic was identical. Why? Because they felt it wasn’t working. And when you stop taking your meds, your condition gets worse. That’s not the drug’s fault. It’s the expectation.
How Doctors Can Fix This
This isn’t a patient problem. It’s a communication problem. Most doctors don’t talk about the placebo effect with generics. They assume patients know the facts. But knowledge doesn’t change belief.There’s a better way. In a 2021 study, doctors who spent just three minutes explaining three things saw nocebo responses drop by 47%:
- "The FDA requires generics to work the same as the brand. They’re held to the same strict standards." (Cite 21 CFR 320.22-24)
- "Some people feel different on generics-not because they’re weaker, but because their brain expects a change." (Acknowledge the feeling without dismissing it)
- "Give it two weeks. If you still feel off, we’ll reassess." (Set a clear, short-term expectation)
That’s it. No jargon. No sales pitch. Just clarity and empathy. Clinicians trained in this method improved generic adherence by 32%. Patients didn’t need to believe in generics. They just needed to believe their doctor wasn’t hiding something.
What Happens When You’re Not Told
Imagine this: You’ve been on brand-name sertraline for anxiety. Your doctor switches you to generic without saying why. You notice your mood feels "off." You think, "It’s the generic. It’s not working." You stop taking it. Your anxiety spikes. You go back to the doctor. They prescribe the brand again. Cost: $150/month instead of $5.This isn’t rare. In antidepressant trials, patients on generic-labeled sertraline dropped out at 22% higher rates than those on brand-labeled versions-even though the pills were identical. The difference? The label. The fear. The unspoken doubt.
And it’s not just antidepressants. Statins, blood pressure meds, thyroid drugs-any long-term treatment where symptoms are subtle or slow to change-falls into this trap. Your brain doesn’t wait for lab results. It waits for how you feel. And if you feel worse, your brain assumes the drug failed.
What You Can Do
You don’t need to wait for your doctor to fix this. You can take control:- Ask your pharmacist: "Is this the same as my old pill?" They’ll confirm it’s bioequivalent.
- Check the FDA’s Generic Drug Facts page. It’s free, clear, and backed by science.
- Track your symptoms for two weeks after switching. Give your body time to adjust to the new mental model.
- If you feel worse, don’t assume it’s the drug. Ask: "Could this be my brain reacting to the change?""
- Don’t switch back unless you’ve talked to your doctor. Reverting to brand just reinforces the belief that generics don’t work.
Some people will still feel different. That’s normal. The brain is wired to notice change. But if you’ve been stable on a brand, switching to a generic doesn’t mean you’re losing control. It means you’re learning to trust a new label.
The Bigger Picture
This isn’t just about your prescription. It’s about a $1.4 billion problem in the U.S. healthcare system every year-money spent on brand-name drugs that aren’t better, just more expensive. That’s money that could pay for more screenings, more mental health visits, more insulin for people who can’t afford it.And it’s not just the U.S. The European Union is funding a €2.4 million project to create standardized patient education on generics. The FDA is now requiring generic manufacturers to keep pill color and shape consistent because changing them increased discontinuation rates by nearly 20%.
The future isn’t about hiding the truth. It’s about framing it right. The pill in your hand is just as powerful as the one you used to take. But your brain needs to know that.
What’s Next?
A digital tool called the "Expectation Modulation Protocol" is being tested right now. It’s a 12-minute video that explains the placebo effect in plain language. In trials, it reduced nocebo responses by 53%. It’s not magic. It’s education. And it’s coming to clinics soon.For now, the best tool you have is information. You don’t need to be a scientist to understand this: Your body responds to more than chemistry. It responds to meaning. And if you’re willing to look at the science, not just the label, you’ll find that the cheapest pill in the bottle can still be the most powerful one-if you let it be.
Are generic drugs really the same as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also deliver the same amount of medicine into your bloodstream within the same time frame-within 80-125% of the brand’s performance. This is called bioequivalence. Thousands of studies confirm they work the same way in the body.
Why do I feel different on a generic drug?
You’re not imagining it-but the difference isn’t chemical. It’s psychological. If you’ve been on a brand-name drug for a long time, your brain has learned to expect a certain level of relief. When you switch to a generic, even if it’s identical, your brain may interpret the change as a loss of effectiveness. This is called the nocebo effect. It’s real, but it’s not caused by the drug itself. Giving yourself two weeks to adjust often helps.
Can the placebo effect make a generic drug work better?
Yes-and it already does. Studies show that when patients believe they’re taking a brand-name drug-even if it’s a placebo-they report stronger pain relief and better symptom control. The same applies to generics: if you believe they work, your brain helps them work. That’s why clear communication from your doctor matters more than the pill’s color or price.
Should I avoid generics because of the placebo effect?
No. Avoiding generics because of fear of reduced effectiveness means paying more for the same medicine. The placebo effect can be managed-not eliminated-by understanding how it works. Most people do just as well on generics once they’re informed. The financial savings are real, and the health benefits are too. Millions of people worldwide take generics successfully every day.
What should I say to my doctor if I think the generic isn’t working?
Say this: "I switched to the generic, and I’m noticing a change in how I feel. I know they’re supposed to be the same, but I’m wondering if it’s my body adjusting or if something else is going on." This opens the door for a conversation, not a dismissal. Your doctor can check your labs, review your symptoms, and help you decide whether to stay on the generic or explore other options.
Is it safe to switch back and forth between brand and generic?
It’s safe from a medical standpoint-both are bioequivalent. But switching back and forth can reinforce the idea that generics don’t work, which can make future switches harder. It also increases costs and risks inconsistent adherence. If you’re having trouble, talk to your doctor first. Don’t switch on your own unless there’s a clear medical reason.
