
Every year, thousands of workers breathe in dust and fibers they never should have been exposed to. By the time they feel the tightness in their chest or the cough that won’t quit, it’s often too late. Silicosis and asbestosis aren’t just rare illnesses-they’re preventable tragedies that keep happening because safety gets overlooked. These aren’t diseases you catch from a virus or bad luck. They’re caused by what you breathe at work. And they don’t go away.
What Silicosis and Asbestosis Actually Do to Your Lungs
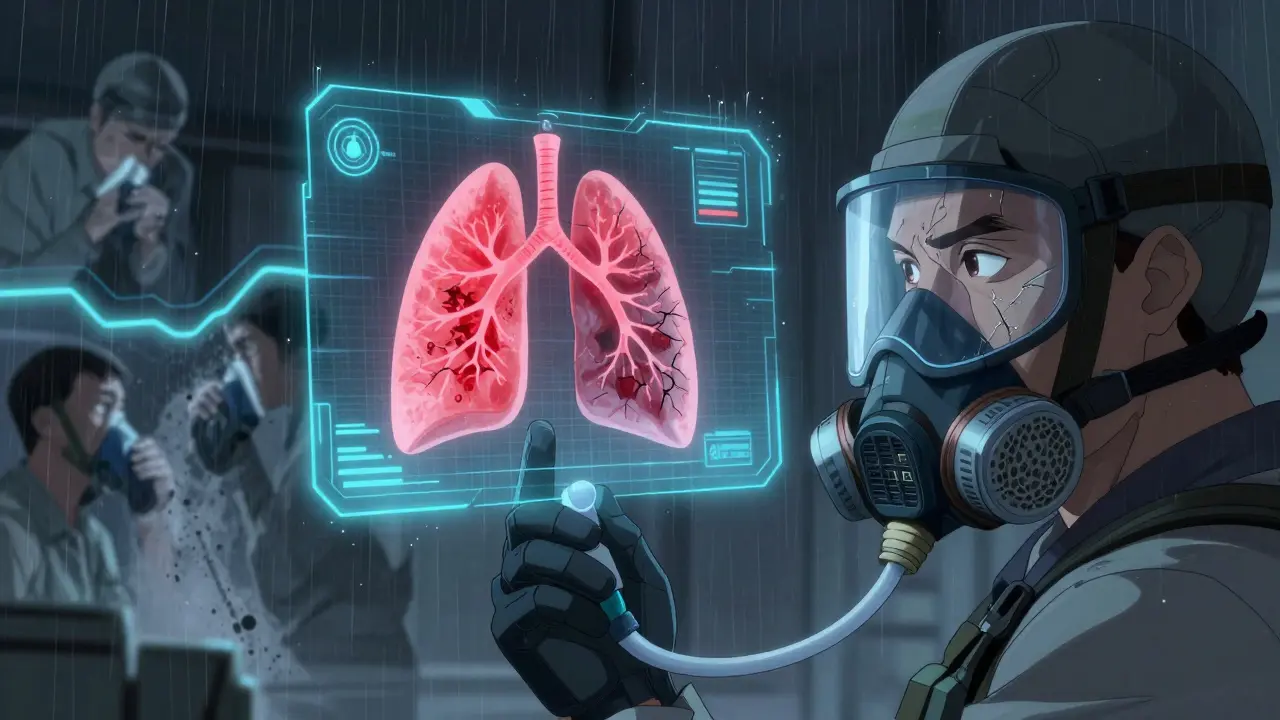
Silicosis comes from breathing in crystalline silica dust. You’ll find it in sand, stone, concrete, and even some ceramics. When workers cut, grind, or drill these materials-especially without water or ventilation-the dust becomes airborne. Tiny particles, smaller than a red blood cell, slip deep into the lungs. The body tries to fight them off, but instead of clearing them, it scars the tissue. Over time, those scars stiffen the lungs. Breathing becomes harder. Eventually, even walking short distances can leave you gasping.
Asbestosis is similar, but it’s caused by asbestos fibers. These fibers are thin, sharp, and durable. They don’t break down in the body. Once inhaled, they stick to lung tissue and trigger chronic inflammation. The lungs thicken and scar, losing their elasticity. People with asbestosis often develop a dry, hacking cough and shortness of breath during simple tasks. Unlike infections, these diseases don’t improve with rest or medicine. Once the damage is done, it’s permanent.
Both conditions can take years to show symptoms. A worker might spend 10, 15, even 20 years on the job before noticing anything wrong. By then, the disease has already advanced. The CDC reports that between 2004 and 2014, over 1,100 U.S. workers died from asbestosis alone. Silicosis killed around 1,200 people each year in the U.S. during that same period. These aren’t numbers from the 1950s. These are recent deaths. And they didn’t have to happen.
The Hierarchy of Control: What Actually Works
There’s a proven order of how to stop these diseases. It’s called the hierarchy of controls. And it’s not just theory-it’s the difference between life and death.
The best solution? Eliminate the hazard. If you can replace silica-containing materials with safer alternatives, do it. Some manufacturers now offer engineered stone with lower silica content. It’s not always possible, but when it is, it’s the most effective step.
Next best? Substitution. Use water instead of dry cutting. Wet cutting reduces silica dust by up to 90%. That’s not a small improvement-it’s game-changing. In construction, a wet saw isn’t just a tool; it’s a lifesaver.
Then comes engineering controls. Local exhaust ventilation (LEV) systems pull dust away at the source. OSHA recommends air velocity between 100 and 150 feet per minute at the point of dust generation. Sealed enclosures that trap 95% of dust are also highly effective. These systems cost between $2,000 and $5,000 per workstation, but the return on investment comes in under two years through fewer workers’ compensation claims and less lost time.
Administrative controls-like limiting exposure time or rotating workers-are helpful, but they only cut exposure by 50-70%. They’re a backup, not a solution.
Finally, there’s personal protective equipment (PPE). Respirators are essential, but they’re the last line of defense. N-95 masks filter 95% of particles 0.3 microns in size. P-100 masks go further-99.97% filtration. But here’s the catch: if the mask doesn’t fit, it’s useless. OSHA requires annual fit testing. Yet, a CDC report found that 68% of worker complaints about respirators were about discomfort or poor fit. Workers in 90-degree heat often remove them. Some even cut the straps to make them easier to wear. That’s not negligence-it’s a system failure.
Why Prevention Still Fails, Even When We Know How
Companies know the rules. OSHA has had a silica standard since 2016. The European Union is tightening asbestos limits by 2025. Yet, violations keep happening. In 2021, OSHA cited over 1,000 construction companies for silica violations-$3.2 million in fines. Why?
One reason? Speed. On a job site, time is money. Wet cutting takes longer. Dust collection systems need maintenance. Fit testing requires scheduling. Some foremen still push workers to “just get it done.” One Reddit user in construction wrote: “My company finally got wet cutting saws last year and silica dust is way down, but the foreman still yells at us for taking too long with water methods.”
Another reason? Small businesses. A Wisconsin study found that 78% of companies with fewer than 20 employees had no formal respiratory protection program. They don’t have safety officers. They don’t have the budget for LEV systems. They rely on masks and hope.
And then there’s culture. If supervisors don’t wear their own respirators, workers won’t either. A blog tracking 15 construction firms found that when managers modeled proper PPE use 100% of the time, respiratory incidents dropped by 65% over three years. Leadership matters. Safety isn’t a poster on the wall-it’s a daily habit.
Monitoring and Early Detection: Catching It Before It’s Too Late
Even with perfect controls, accidents happen. That’s why health monitoring is non-negotiable.
Spirometry tests measure how well your lungs are working. They’re simple, quick, and cheap. The American Thoracic Society recommends baseline testing when someone starts a job with respiratory hazards, then every five years. For those with existing conditions or higher exposure, annual testing is critical.
Why? Because symptoms often appear only after significant damage. A worker might think their shortness of breath is just from getting older. But spirometry can detect early decline-before the cough starts, before the fatigue sets in. Studies show early intervention can slow disease progression by 30-50%.
And it’s not just about lung function. Regular check-ups give workers a chance to speak up. If someone says, “I’ve been coughing more since we started cutting stone,” that’s a red flag. A good program doesn’t punish those who report symptoms-it protects them.
The Bigger Picture: Why This Matters Beyond the Job Site
Occupational lung diseases make up 15-20% of all work-related illnesses in the U.S. Construction, mining, and manufacturing account for 75% of cases. But the ripple effect goes beyond the worker.
When a 52-year-old bricklayer can’t climb stairs without stopping, his family takes on more care. Medical bills pile up. He can’t play with his grandkids. He might retire early-or worse, die young. The global market for respiratory protection is growing fast-projected to hit $11.3 billion by 2027. That’s not just a business opportunity. It’s a sign that people are finally waking up.
But money isn’t the answer. Culture is. The European Respiratory Society wants to eliminate these diseases by 2030. NIOSH launched a free digital tool called “Prevent eTool” in 2023. Companies using it saw a 40% drop in respiratory incidents within six months. The technology exists. The science is clear.
The only thing missing is the will to enforce it.

What Workers and Employers Can Do Right Now
If you’re a worker:
- Ask if your job involves silica or asbestos. If you’re cutting, grinding, or demolishing concrete, stone, or old insulation, you’re at risk.
- Insist on a proper respirator fit test. If you’ve never had one, ask for it. It’s your right under OSHA.
- Report unsafe conditions without fear. OSHA’s whistleblower protections are real. Use them.
- Don’t smoke. Smoking doubles your risk of developing severe lung disease when exposed to silica or asbestos.
If you’re an employer:
- Install wet cutting systems and local exhaust ventilation. Don’t wait for OSHA to show up.
- Train your team properly. Four to six hours of initial training, not the bare minimum two. Make it real. Show videos. Let workers ask questions.
- Store respirators in clean, dry containers. A dirty mask is worse than no mask.
- Lead by example. Wear your PPE every day. No exceptions.
- Start spirometry testing. It’s not expensive. It’s not complicated. But it saves lives.
The truth is simple: silicosis and asbestosis don’t have to exist. We have the tools. We have the knowledge. We just need to use them-consistently, without compromise.
Can you get silicosis from one-time exposure to silica dust?
While silicosis usually develops after years of exposure, extremely high levels of silica dust-like from an explosion or uncontrolled sandblasting-can cause acute silicosis in weeks or months. This is rare but deadly. Even short-term exposure to large amounts of dust can damage the lungs permanently.
Is asbestosis the same as mesothelioma?
No. Asbestosis is scarring of the lung tissue caused by asbestos fibers. Mesothelioma is a cancer of the lining of the lungs, heart, or abdomen. Both are caused by asbestos exposure, but they’re different diseases. One is a scarring condition; the other is cancer. Both are fatal. Neither has a cure.
Are N-95 masks enough for silica or asbestos?
N-95 masks filter 95% of particles, but they’re not always sufficient for high-risk tasks like demolition or abrasive blasting. P-100 respirators filter 99.97% of particles and are required in high-exposure environments. N-95s may be acceptable for low-level, short-term tasks-but only if fit-tested and used correctly.
Can you still work if you have silicosis or asbestosis?
You can, but you shouldn’t. Continuing exposure will make the disease worse faster. Once diagnosed, the priority is to stop all further exposure. Many workers qualify for disability benefits or job reassignment. Staying in a dusty environment after diagnosis is like pouring gasoline on a fire.
Why don’t more companies use wet cutting or ventilation systems?
Cost and convenience. Some employers think masks are cheaper than installing ventilation. But when you factor in workers’ compensation claims, lost productivity, and fines, engineering controls pay for themselves in under two years. The real cost isn’t money-it’s the failure to prioritize human health over speed.
Is there a cure for silicosis or asbestosis?
No. There is no cure. Once the lung tissue is scarred, it doesn’t heal. Treatment focuses on managing symptoms-oxygen therapy, pulmonary rehab, quitting smoking, and avoiding further exposure. The only way to truly prevent these diseases is to stop the exposure before it starts.
What Comes Next?
Technology is getting better. Wearable sensors now give real-time dust readings. AI tools can predict exposure risks based on job tasks. But tools don’t change culture. People do.
The next step isn’t more regulations. It’s more accountability. Employers who ignore safety aren’t just breaking rules-they’re breaking trust. Workers who speak up aren’t being difficult-they’re being brave.
If you’re reading this and you work with dust or fibers, ask yourself: Is my safety being treated like a priority-or an afterthought? The answer might save your life.

Patty Walters
January 9, 2026 AT 20:26just had a guy at work ask me why we bother with wet cutting when he's got an n95 on... i showed him the fit test results from last year. 80% of his masks were leaking. he stopped complaining after that. safety ain't about gear, it's about doing it right.
Johanna Baxter
January 11, 2026 AT 00:15my cousin died from this. they told him it was 'just a cough' for 3 years. by the time they found out, his lungs were stone. no one held anyone accountable. just another number.
Diana Stoyanova
January 11, 2026 AT 11:01listen. i used to work demolition. we didn't have wet saws. we had dust clouds you could see in the sun. i thought i was tough. turns out i was just dumb. now i train new hires. i show them the x-rays. i tell them: 'your grandkids won't care how fast you finished the job. they'll remember if you were there to see them graduate.' it hits harder than any OSHA poster. safety isn't a policy-it's a promise.
Jenci Spradlin
January 12, 2026 AT 21:50psst-p-100s are overkill for light stuff. n95s work fine if they're fit tested and changed daily. i've seen too many guys wear a p-100 for 3 days straight, sweat through it, then blame the mask. it's not the gear, it's the habit.
Kiruthiga Udayakumar
January 13, 2026 AT 14:15in india, we still use hand tools to cut stone. no water. no masks. no training. workers breathe dust for 12 hours a day and get paid $5. this isn't just negligence-it's exploitation. why do rich countries care only when it's their own people? the world needs to wake up.
Phil Kemling
January 15, 2026 AT 06:13we treat work-related illness like a personal failure-'why didn't you wear your mask?'-but the system is designed to make compliance hard. time pressure, cost cuts, no oversight. it's not about willpower. it's about structure. if we want fewer deaths, we need to redesign the work, not blame the worker.
Heather Wilson
January 16, 2026 AT 15:59the real problem? people think this is a 'health issue.' it's not. it's a moral failure disguised as economics. companies spend millions on marketing and nothing on lung protection. and we call this capitalism? this isn't free enterprise-it's legalized murder with a 401(k).
Matthew Maxwell
January 17, 2026 AT 19:26you people act like this is new. silica exposure has been killing people since the 1930s. the solution has been known for 80 years. yet here we are. this isn't ignorance-it's willful indifference. if your boss won't act, file a complaint. don't wait for your lungs to fail. you're not a martyr. you're an employee. demand safety. or leave.
Ashley Kronenwetter
January 17, 2026 AT 23:46as someone who works in occupational health, I've reviewed over 200 cases of silicosis. Every single one was preventable. The data doesn't lie. What’s frustrating is not the science-it’s the refusal to act. We have the tools. We have the evidence. What we lack is the collective will to prioritize life over profit. This isn't a debate. It's a duty.
Elisha Muwanga
January 19, 2026 AT 16:51why do we keep letting foreign countries get away with this? we enforce safety here, but let contractors from overseas bring their unsafe practices in? that’s not global progress-that’s hypocrisy. if you want to work here, you follow our rules. no exceptions. no loopholes. no excuses.