When you start a new medication, especially one with serious side effects, it’s not enough to just take it and hope for the best. Some drugs can quietly damage your liver, drop your white blood cell count, or throw your electrolytes out of balance-before you even feel sick. That’s where a lab monitoring calendar comes in. It’s not a fancy app or a doctor’s suggestion you can ignore. It’s your lifeline to catching problems early, before they become emergencies.
Why Lab Monitoring Isn’t Optional
Not every medication needs blood tests. But for others, skipping a single lab check can mean the difference between a minor tweak and a hospital visit. Take clozapine, used for treatment-resistant schizophrenia. It can cause agranulocytosis-a dangerous drop in white blood cells that leaves you defenseless against infections. Without weekly blood tests for the first few months, you’re flying blind. Even after things stabilize, you still need checks every few weeks for life. No exceptions. Lithium, a common mood stabilizer for bipolar disorder, is another example. It’s effective-but the gap between a therapeutic dose and a toxic one is tiny. If you don’t get your blood levels checked 5 to 7 days after starting it, and then regularly after that, you could end up with tremors, confusion, or even kidney damage. These aren’t rare cases. They’re predictable. And they’re preventable. Warfarin, a blood thinner, demands monthly INR tests. If your INR is too high, you risk internal bleeding. Too low, and you’re not protected from clots. A missed test? That’s not just negligence-it’s a ticking clock.What Gets Monitored and When
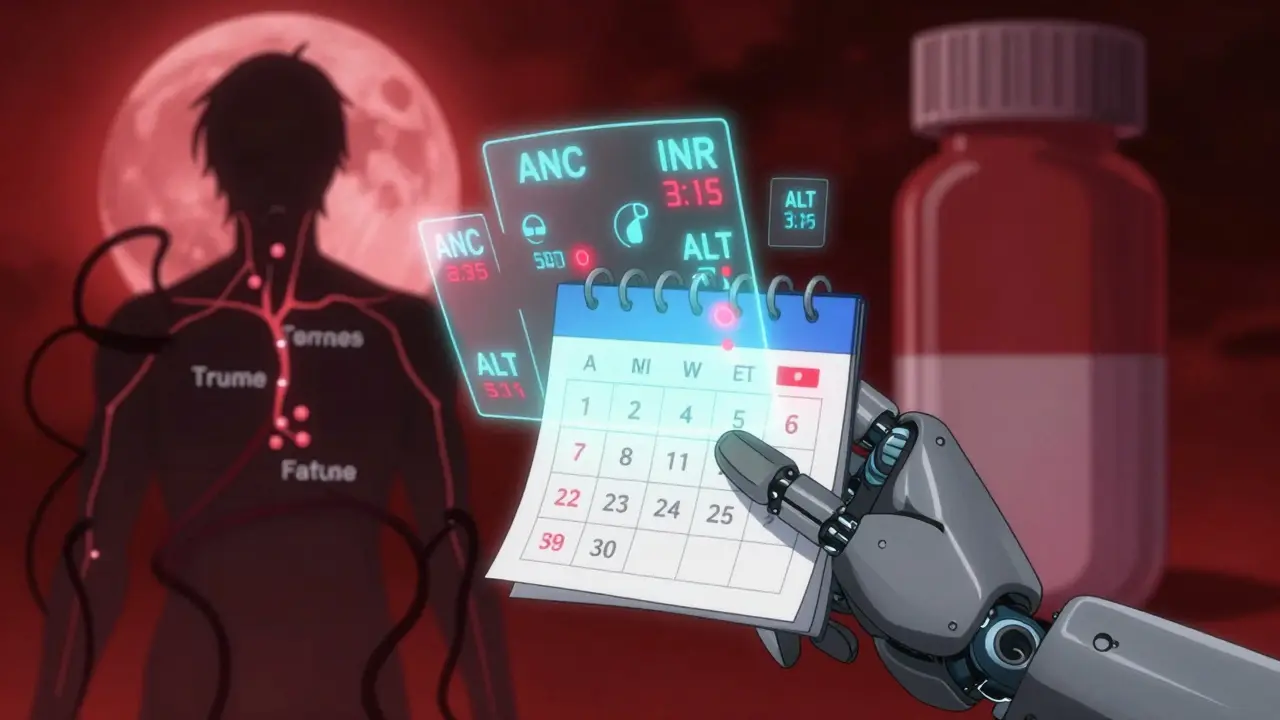
Different drugs need different checks. There’s no one-size-fits-all. Here’s what you’re likely to see based on your medication:- Clozapine: Weekly ANC (absolute neutrophil count) for the first 18 weeks, then every two weeks, then monthly. If your ANC drops below 500/μL, you stop the drug immediately.
- Lithium: Blood levels checked 5-7 days after starting, then weekly until stable. After that, at least every 6 months-more often if you’re older, dehydrated, or on other meds.
- Warfarin: Monthly INR. More frequent if your dose changes, you start antibiotics, or you change your diet (especially leafy greens).
- Statins: Liver enzymes (ALT, AST) checked before starting and again after 3 months. If normal, every 6-12 months.
- Corticosteroids (used over 2 weeks): Morning cortisol test to check for adrenal suppression. This isn’t optional if you’ve been on prednisone for more than a month.
- Anticonvulsants (like valproate): Liver function, ammonia levels, and CBC every 3-6 months. These drugs can silently harm your liver or pancreas.
- LONSURF (cancer therapy): Weekly blood counts for neutrophils and platelets. Also track diarrhea, nausea, and fatigue daily. Dose delays happen fast if counts drop too low.
Some drugs need more than blood tests. Glaucoma medications like dorzolamide/timolol require annual eye exams. Antipsychotics like olanzapine need yearly metabolic panels-blood sugar, cholesterol, weight-to catch diabetes and weight gain early.
Digital vs. Paper Calendars: What Works
You can track your labs on paper, in a phone app, or through your doctor’s electronic health record. Each has pros and cons.Printable templates (like those from Community Behavioral Health or CBH Philly) are simple. You print them, fill them out by hand, and bring them to appointments. They’re reliable, don’t need batteries, and work for people who don’t use smartphones. But they don’t remind you. You have to remember to update them. Miss a week? You’re back to guessing.
Digital tools like Blood Cancer United’s Health Manager app do more than remind you. They let you log side effects-headache, fatigue, nausea-alongside your lab results. Over time, the app shows patterns: “Your platelets always drop 3 days after your dose.” “Your blood sugar spikes after eating pasta on weekends.” That kind of insight helps your doctor adjust your treatment, not just react to numbers.
Ulta Lab Tests lets you order your own blood work, which sounds great-but without a doctor’s interpretation, you might panic over a slightly high ALT or miss a critical trend. Lab results mean nothing without context. Don’t order tests on your own unless you have a plan to review them with your provider.
The best systems sync with your medication schedule. LONSURF’s official calendar, for example, links each dose to the exact lab tests you need that week. It even tracks missed doses and temperature spikes-key signs of infection when your immune system is down.
How to Build Your Own Lab Monitoring Calendar
Start with what your doctor gives you. Then make it your own.- Write down every test your provider says you need, with the frequency. Don’t assume you’ll remember. Write it.
- Mark the dates on a physical calendar or digital one (Google Calendar, Apple Health). Set a recurring reminder 3 days before each test.
- Link side effects to timing. Did you feel dizzy every time you took your pill at 8 p.m.? Did your headache start after you ate pizza? Note it. Patterns matter.
- Update it every time your dose changes. More pills? New drug? Add the new tests immediately. Don’t wait for your next appointment.
- Bring it to every visit. Even if your doctor says they have your records, they’re busy. A clear, updated calendar saves time and prevents mistakes.
Pro tip: Keep a small notebook in your wallet or phone case with your key lab dates and contact info for your pharmacy and lab. If you’re in a rush or forget your main calendar, this backup can prevent a missed test.
Common Mistakes That Put You at Risk
People skip lab monitoring for all the wrong reasons:- “I feel fine.” That’s the whole point. Side effects don’t always cause symptoms until it’s too late.
- “It’s too expensive.” Many labs are covered by insurance. If cost is an issue, ask your pharmacist about patient assistance programs. A single hospital visit for a preventable complication costs thousands.
- “I forgot.” Set three reminders: 7 days, 3 days, and the day before. Use different methods-phone, text, alarm. Don’t rely on memory.
- “My doctor didn’t remind me.” Doctors are overwhelmed. It’s not their job to chase you down. You’re the one taking the drug. You’re the one who needs to stay on top of it.
And don’t assume your pharmacist will call you. They might, but they’re not responsible for your monitoring schedule. That’s yours.
What Happens If You Skip a Test?
Skipping one lab test doesn’t mean disaster. But it opens the door.With clozapine, one missed ANC test could mean you don’t catch a drop in white cells until you’re already sick with a fever. By then, you might need hospitalization, IV antibiotics, and weeks off the drug. You lose control of your treatment.
With lithium, one skipped check could mean your levels have crept up over weeks. You start feeling sluggish, your hands shake, your speech slurs. Then you vomit. Then you have a seizure. That’s lithium toxicity. It’s rare-but it’s preventable with a simple blood test.
With warfarin, one missed INR could mean you’re bleeding internally and don’t know it. A headache that won’t go away? A bruise that spreads? That’s not normal. That’s a warning.
These aren’t hypotheticals. They happen every day. And they’re avoidable.
What’s Next? The Future of Monitoring
The future is smarter calendars. Some apps now sync with wearables-tracking heart rate, sleep, and activity-then cross-referencing them with your lab results. If your resting heart rate spikes and your platelets drop the same week, the app flags it before you even feel unwell.AI tools are starting to predict risks based on your history. If your last three ANC values dropped 10% each month, the system might suggest moving your next test up by a week. That’s not science fiction-it’s already in trials.
But for now, the best tool is still the one you use consistently: a simple, clear calendar you update yourself. No app, no AI, no reminder system replaces personal responsibility.
Final Thought: You’re the Boss of Your Body
Medications save lives. But they also carry risks. Your job isn’t just to take the pill. It’s to understand the consequences. To track the numbers. To notice the changes. To speak up when something feels off.Lab monitoring calendars aren’t bureaucracy. They’re your armor. Use them. Update them. Protect yourself.
Do I really need a lab calendar if my doctor says I’m fine?
Yes. Doctors rely on data, not how you feel. Many dangerous side effects-like low white blood cells, liver damage, or electrolyte imbalances-don’t cause symptoms until they’re serious. Your calendar gives your doctor the evidence they need to keep you safe, not just assume everything’s okay.
Can I skip lab tests if I’m feeling good on my medication?
No. Feeling good doesn’t mean your body is fine. Medications like clozapine, lithium, and warfarin can cause internal damage without you noticing. Your blood test is the only way to see what’s happening inside. Skipping tests is like driving with your eyes closed because the road feels smooth.
What if I can’t afford the lab tests?
Many insurance plans cover required monitoring. If you’re uninsured or underinsured, ask your pharmacist or doctor about patient assistance programs. Pharmaceutical companies often offer free or low-cost testing for medications like clozapine or LONSURF. Don’t skip tests because of cost-ask for help instead.
How do I know which tests I need for my specific drug?
Your prescribing doctor or pharmacist should give you a written plan when you start the medication. If they didn’t, ask: “What blood tests do I need, how often, and why?” Reliable sources like the NIH, FDA, or drug manufacturer guidelines (e.g., Taiho Oncology for LONSURF) also list standard monitoring requirements. Don’t guess-get the facts.
Should I use an app or a paper calendar?
Use whatever works for you. Apps like Health Manager help track side effects and patterns over time. Paper calendars are reliable and don’t need charging. The key isn’t the tool-it’s consistency. If you’ll actually use it, that’s the right choice. Just make sure you bring it to every appointment.
What if I miss a lab test? Can I just reschedule?
Yes, reschedule-but don’t delay. Missing one test doesn’t mean you’re in danger yet, but it does mean you’re flying blind. Contact your provider right away. If your drug requires strict timing (like lithium levels needing 12 hours post-dose), make sure the new test is scheduled at the correct time. Don’t wait until your next routine visit.
Do I still need monitoring if I’ve been on the same dose for years?
Yes. Your body changes. Your kidneys, liver, and metabolism aren’t the same at 50 as they were at 30. Other medications you take can interact. Even small changes in diet, hydration, or sleep can affect how your body handles the drug. Lifelong monitoring isn’t about suspicion-it’s about staying safe as you age.

Nancy Kou
December 20, 2025 AT 07:13This is the kind of post that should be mandatory reading for anyone on long-term meds. I’ve seen friends ignore lab checks because they ‘felt fine’-then end up in the ER with liver failure from statins. No one tells you how silent these dangers are until it’s too late. This isn’t fearmongering-it’s survival.
Hussien SLeiman
December 20, 2025 AT 17:16Look, I get it-lab calendars sound like a chore. But let’s be real: if your doctor didn’t emphasize this, they’re either overwhelmed or didn’t care enough to explain. I’ve been on lithium for 12 years. I missed one test because I was ‘too busy.’ Three weeks later, I was shaking so bad I couldn’t hold a coffee cup. Turned out my levels were at 1.8-danger zone. Now I have a sticky note on my mirror. Every. Single. Week. No excuses. If you’re not tracking, you’re gambling with your organs.
Guillaume VanderEst
December 20, 2025 AT 23:36So I just got prescribed clozapine last month. My psychiatrist gave me a 3-page printout with dates and labs. I laminated it. I put it in my wallet. I set alarms on my phone, my watch, and my smart speaker. I even told my mom to call me every Tuesday at 9 a.m. because I forget everything. And you know what? I still almost missed last week’s ANC. This isn’t just advice-it’s a full-time job. But honestly? I’d rather do the work than wake up in ICU because I was too lazy to check a number.
Alisa Silvia Bila
December 22, 2025 AT 17:32My dad was on warfarin for years. He kept a notebook. Every INR, every dose, every time he ate kale. He didn’t trust apps. Said they glitch. He was right-once his phone died and he forgot his numbers. But his notebook saved him. He brought it to every appointment. Doctors loved him. He lived to 87. Simple tools, done consistently, beat fancy tech every time.
Janelle Moore
December 22, 2025 AT 20:31Wait… so you’re telling me the government and Big Pharma want us to do all these tests so they can keep us dependent? What if the labs are rigged? What if they’re just trying to make us pay for unnecessary blood draws? I read online that lithium causes kidney damage because the FDA is in cahoots with pharma. And don’t get me started on how they manipulate INR ranges to sell more anticoagulants. I stopped all my meds and started drinking apple cider vinegar. My ‘levels’ are perfect now. You’re being manipulated.
Henry Marcus
December 23, 2025 AT 07:22Okay, but have you ever stopped to think-what if the ‘normal’ lab ranges are lies? What if the ‘safe’ thresholds were set by drug companies to maximize profit? I did my own blood work through Ulta-my ALT was 48. The ‘normal’ range says 0–40. But I found a Reddit thread where a guy in Germany said his liver enzymes are naturally 60 and he’s 92 and still hikes mountains. Who defines ‘normal’? The FDA? The AMA? Or the guys who own the test kits? I’m not trusting their numbers anymore. I’m listening to my body. And my body says: ‘Stop the tests. Stop the pills.’
Carolyn Benson
December 24, 2025 AT 10:44It’s fascinating how we’ve been conditioned to believe that medicine is a science when it’s really a ritual. We submit our blood to strangers in white coats, then trust their numbers like sacred scripture. But what if the ‘danger’ is manufactured? What if the real toxicity isn’t in the drug-but in the fear? I stopped my monitoring. I stopped checking. And guess what? I felt freer. Not because I was reckless-but because I stopped outsourcing my body’s authority to institutions that profit from my anxiety. Maybe the calendar isn’t armor. Maybe it’s a cage.
Chris porto
December 25, 2025 AT 09:06I think this post is really important, but I also think we need to talk about the emotional weight of this. It’s not just about remembering dates-it’s about living with constant vigilance. I’ve been on anticonvulsants for 15 years. Every 3 months, I feel this dread walking into the lab. Like my body is a ticking bomb and I’m the only one holding the detonator. It’s exhausting. Maybe we need more support systems-not just calendars, but community. People who get it. Who don’t judge you for forgetting once. Who remind you without shaming you. Because this isn’t just medical-it’s psychological.
William Liu
December 25, 2025 AT 13:03Just started clozapine last week. I was scared. But I printed the calendar, taped it to my fridge, and set a daily alarm. I’m not perfect-I missed Tuesday’s test-but I called my pharmacist immediately and got it rescheduled. It’s not about being flawless. It’s about showing up. And honestly? Doing this feels like the most powerful thing I’ve done for myself in years. You’re not just taking a pill. You’re choosing to live. Keep going.
Aadil Munshi
December 26, 2025 AT 18:00Let me break this down for you like you’re five: If you’re on meds that require labs, you’re not a patient-you’re a data point. The system wants you to think you’re in control, but really, you’re just a cog in a machine that makes money off your compliance. You think you’re protecting yourself? You’re just feeding the cycle. The calendar isn’t armor-it’s a leash. And the only real freedom is to question why you need this system at all. Maybe the real solution isn’t tracking your blood-but rejecting the idea that your body needs permission to be healthy.
Erica Vest
December 28, 2025 AT 13:52For anyone on clozapine or lithium: your doctor should have given you a written monitoring schedule at initiation. If they didn’t, ask for it. The FDA-mandated guidelines for clozapine are publicly available on the REMS website. For lithium, the British National Formulary recommends baseline, then weekly until stable, then every 3–6 months. Always confirm your lab window-lithium levels must be drawn 12 hours post-dose. Don’t rely on memory. Don’t assume. Document. Ask. Repeat. This isn’t opinion. It’s protocol. And it saves lives.