
When someone has a seizure, it can be terrifying - not just for the person experiencing it, but for everyone around them. A sudden loss of control, stiffening limbs, staring blankly, or jerking movements - these aren’t just random events. They’re signals from the brain, and understanding them is the first step toward managing epilepsy effectively. Epilepsy isn’t one condition. It’s a group of disorders defined by recurrent, unprovoked seizures. And how we classify those seizures has changed dramatically in the last few years, making it easier for doctors to treat them - if they’re using the latest guidelines.
What Counts as Epilepsy?
You don’t get diagnosed with epilepsy after one seizure. That’s important. A single seizure can happen for many reasons - low blood sugar, a head injury, alcohol withdrawal, or even extreme sleep deprivation. Epilepsy means your brain has a lasting tendency to have seizures without an immediate trigger. According to the International League Against Epilepsy (ILAE), you’re diagnosed with epilepsy if you’ve had at least two unprovoked seizures more than 24 hours apart. Or, if you’ve had one seizure and there’s a 60% or higher chance of another one happening within the next 10 years. That’s based on things like brain scans showing scarring, or EEG patterns that look like epilepsy even between seizures.
Worldwide, about 50 million people live with epilepsy. In the U.S., that’s 3.4 million. And every year, 5 million new cases are diagnosed. Many of these cases go undiagnosed for years - especially in rural areas or low-income countries where EEG machines and neurologists are hard to find. The average time from first seizure to correct diagnosis? About 2.3 years. That’s a long time to be afraid of the next episode.
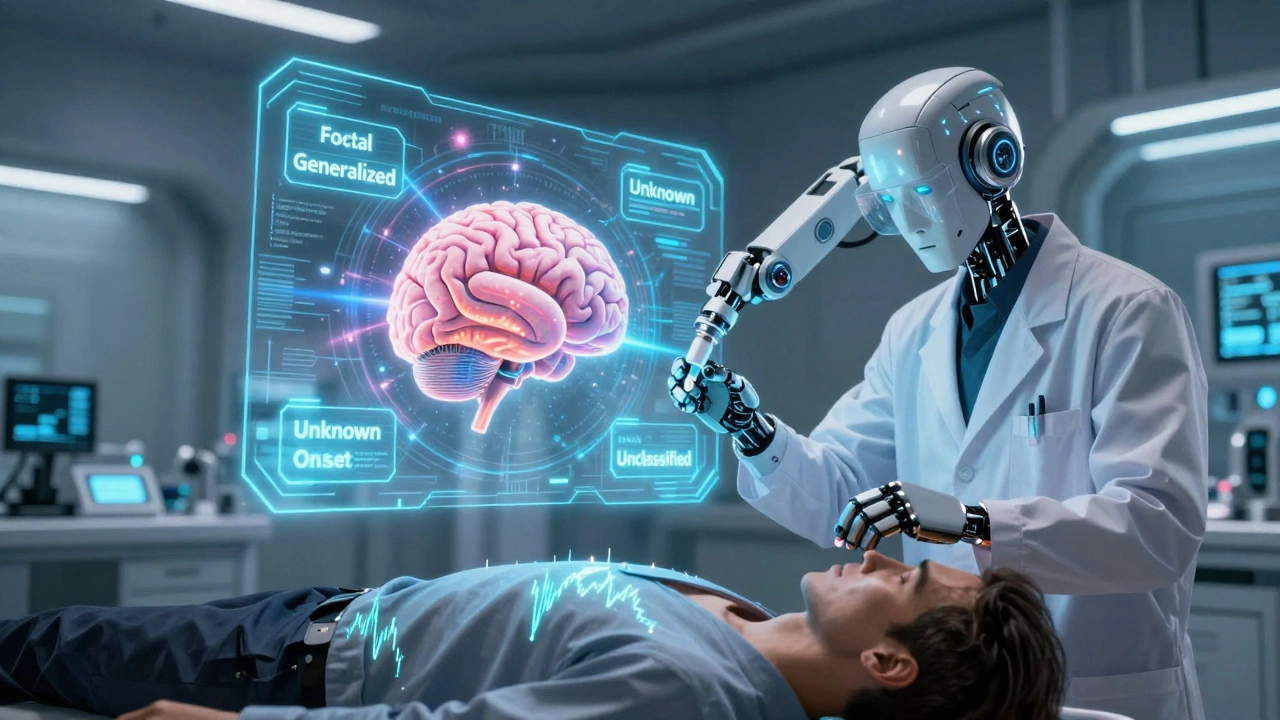
The New Way to Classify Seizures (2025 Update)
In 2025, the ILAE updated its seizure classification system - and this time, they listened to doctors. The old system had over 60 different seizure names. Too many. Too confusing. The new system cuts that down to just 21 types. The goal? Make it faster and more accurate for clinicians - even those without deep neurology training.
Seizures are now grouped into four main categories:
- Focal seizures - start in one part of the brain
- Generalized seizures - involve both sides of the brain from the start
- Unknown onset - you don’t know where it started
- Unclassified - not enough information yet
For focal seizures, the big change is in how we talk about awareness. Instead of calling them “simple partial” or “complex partial,” we now say:
- Focal aware seizures - you’re fully awake and aware during it. You might feel a strange smell, see flashing lights, or get a rising feeling in your stomach. No loss of consciousness.
- Focal impaired awareness seizures - you stare blankly, don’t respond, maybe fumble with your clothes. This used to be called “complex partial.” It’s the most common type of focal seizure, making up about 75% of cases.
Generalized seizures are simpler now, too. The main types are:
- Absence - brief staring spells, often in kids. Lasts 5-10 seconds. You might blink or flutter your eyelids.
- Myoclonic - sudden jerks, like an electric shock. Usually in the arms or shoulders.
- Tonic - muscles stiffen. Often happens during sleep.
- Clonic - rhythmic jerking, usually in the face or limbs.
- Tonic-clonic - the classic “grand mal” seizure. Stiffening, then shaking, often with loss of bladder control or biting the tongue.
- Atonic - sudden loss of muscle tone. You drop like a puppet with cut strings. Dangerous if you’re standing.
One big shift: doctors now describe seizures by the full sequence of what happens - not just the first sign. A seizure might start with a strange feeling (non-observable), then turn into arm jerking (observable), then end with confusion. That sequence matters for figuring out where it started.
What Triggers Seizures?
Not all seizures happen for no reason. Even if you have epilepsy, certain things can make them more likely. These are triggers - not causes. You can’t cure epilepsy by avoiding triggers, but you can reduce how often they happen.
Common triggers include:
- Sleep deprivation - the #1 trigger for most people. Pulling an all-nighter can set off a seizure the next day.
- Alcohol and drug use - especially binge drinking or quitting cold turkey. Even some over-the-counter cold meds can interfere with seizure meds.
- Flashing lights - only affects about 3% of people with epilepsy. But it’s real. Video games, strobe lights, or even sunlight flickering through trees can trigger them.
- Stress and anxiety - emotional stress spikes cortisol, which can lower your seizure threshold.
- Hormonal changes - many women with epilepsy have more seizures around their period. This is called catamenial epilepsy.
- Missed medication - skipping even one dose can be enough. That’s why pill organizers and phone alarms are non-negotiable.
One surprising trigger? Low blood sugar. People with diabetes or those on strict diets need to watch this. A 2023 study in Epilepsy & Behavior found that 18% of patients with focal seizures reported low glucose as a trigger.
Antiepileptic Medications: How They Work and What to Expect
There are over 25 FDA-approved antiepileptic drugs (AEDs). No single drug works for everyone. The choice depends on seizure type, age, gender, other health conditions, and even lifestyle.
Here are the most commonly prescribed ones:
- Levetiracetam (Keppra) - used for focal and generalized seizures. Often first-line because it’s well-tolerated. Side effects: mood changes, drowsiness.
- Lamotrigine (Lamictal) - good for absence and focal seizures. Also used in bipolar disorder. Risk: serious skin rash if dose is increased too fast.
- Valproate (Depakote) - very effective for generalized seizures, especially myoclonic and absence. But it’s not safe for women who could get pregnant - it can cause birth defects.
- Carbamazepine (Tegretol) - classic for focal seizures. Works well, but interacts with many other drugs. Needs regular blood tests.
- Clobazam (Onfi) - a benzodiazepine. Used for Lennox-Gastaut syndrome. Can cause drowsiness and tolerance over time.
- Topiramate (Topamax) - used for focal and tonic-clonic seizures. Can cause weight loss and kidney stones.
It often takes trying 2 or 3 meds before you find one that works. About 30% of people with epilepsy don’t respond fully to the first drug. That’s why doctors don’t give up quickly. Newer drugs like cenobamate and fenfluramine are now approved for hard-to-treat cases, especially Dravet syndrome.
Side effects are common - dizziness, fatigue, brain fog, weight gain. But many improve after a few weeks. The key is to start low and go slow. Never stop a seizure medication cold turkey. That can trigger status epilepticus - a life-threatening seizure that won’t stop.
What About Surgery and Other Treatments?
Medication isn’t the only option. If seizures keep happening despite two or three drugs, it’s time to consider other paths.
Surgery - if seizures start in one small area of the brain (like the temporal lobe), removing that part can cure epilepsy in up to 70% of cases. A 2024 study in The Lancet showed 68% of patients remained seizure-free five years after surgery.
Neurostimulation - devices like the vagus nerve stimulator (VNS) or responsive neurostimulation (RNS) send small electrical pulses to the brain to stop seizures before they start. These don’t cure epilepsy, but they cut seizure frequency by 50% or more in most patients.
Special diets - the ketogenic diet (high fat, very low carb) has been used for decades in kids with drug-resistant epilepsy. It works by changing how the brain uses energy. Newer versions, like the modified Atkins diet, are easier to follow.
Cannabidiol (CBD) - Epidiolex, a purified CBD oil, is FDA-approved for two rare forms of epilepsy: Dravet syndrome and Lennox-Gastaut syndrome. It doesn’t make you “high.” Studies show it reduces seizures by 30-40% in these patients.

Why Classification Matters - Real Impact
Getting the seizure type right isn’t just academic. It changes your life.
Wrong classification = wrong medication. A 2023 study found that 27% of people were prescribed the wrong drug because their seizure type was misdiagnosed. For example, giving carbamazepine to someone with absence seizures can make them worse. That’s dangerous.
Accurate classification also affects insurance. In the U.S., Medicaid and Medicare reimbursements for epilepsy care depend on correct diagnosis codes. One 2023 report showed that patients with properly classified epilepsy had 29% better access to specialist care and medications.
And it affects your future. If you have focal epilepsy, you might be allowed to drive after 6 months seizure-free. If you have generalized epilepsy, rules are stricter. Some jobs - like commercial driving or working at heights - are off-limits depending on your seizure type and control.
Patients who understand their classification are more likely to stick with treatment. A 2023 study showed that people who could explain their seizure type to their doctor had 34% higher medication adherence. That’s huge.
What’s Next?
The future of epilepsy care is getting smarter. AI tools are being developed to help doctors classify seizures from video recordings - even without EEG. A beta version released in mid-2025 improved diagnostic accuracy by 18% for non-specialists.
Genetic testing is also becoming part of the picture. Some forms of epilepsy are caused by single gene mutations. Identifying them can lead to targeted treatments. For example, patients with SCN1A mutations respond better to sodium channel blockers - and worse to others.
By 2030, experts predict most epilepsy diagnoses will combine clinical history, EEG, brain imaging, and genetic data. The goal? Move from treating seizures to preventing them before they start.
For now, the best thing you can do is get the right diagnosis. If you or someone you know has had a seizure, don’t wait. See a neurologist. Get an EEG. Bring a witness. Write down what happened. The more detail, the better the chance of getting the right treatment - and the right life back.
Can you outgrow epilepsy?
Yes, especially in children. About 70% of kids with epilepsy outgrow it by adulthood, particularly if they have syndromes like benign rolandic epilepsy or childhood absence epilepsy. For adults, the chance of remission is lower - around 30-40% after 10 years of being seizure-free on medication. But remission doesn’t mean cure. The brain’s tendency may still be there, and seizures can return if meds are stopped too soon.
Do all seizures involve convulsions?
No. In fact, most seizures don’t. Focal aware seizures might just feel like a weird smell or a sudden fear. Impaired awareness seizures can look like daydreaming - staring, blinking, or fumbling with clothes. Absence seizures in kids are often mistaken for inattention. Only about 20% of seizures involve full-body shaking. The rest are subtle, which is why they’re often missed or misdiagnosed.
Can stress cause epilepsy?
Stress doesn’t cause epilepsy, but it can trigger seizures in people who already have it. Chronic stress raises cortisol levels, which lowers the brain’s seizure threshold. In some cases, extreme psychological trauma can lead to psychogenic non-epileptic seizures (PNES), which look like epileptic seizures but aren’t caused by abnormal brain electricity. These require different treatment - usually therapy, not medication.
Are antiepileptic drugs addictive?
Most antiepileptic drugs are not addictive. Unlike benzodiazepines (like Xanax or Valium), they don’t create a craving or euphoria. However, stopping them suddenly can cause rebound seizures or even status epilepticus - which is why you must taper off under medical supervision. Some people feel dependent on them because they rely on the medication to prevent life-altering seizures, but that’s not addiction - it’s medical necessity.
Can you drive with epilepsy?
It depends on your seizure type, control, and local laws. In Australia, you must be seizure-free for 6 months (or 3 months if only having nocturnal seizures) before driving again. Rules vary by state. In the U.S., it’s state-by-state - from 3 months to 1 year. If your seizures are controlled with medication and you follow your doctor’s advice, driving is usually possible. But if you have frequent generalized seizures or uncontrolled focal seizures with impaired awareness, driving is typically restricted for safety reasons.
What should you do if someone is having a seizure?
Stay calm. Time the seizure. If it lasts more than 5 minutes, call emergency services. Don’t put anything in their mouth - that’s a myth and can cause injury. Gently turn them onto their side to keep their airway clear. Remove nearby objects. Don’t hold them down. After the seizure, stay with them until they’re fully awake. They may be confused, tired, or have a headache. Offer water if they’re alert. If it’s their first seizure, or if they’re injured, pregnant, or have diabetes, get medical help immediately.

Emmanuel Peter
December 5, 2025 AT 17:19Ashley Elliott
December 6, 2025 AT 11:21Chad Handy
December 8, 2025 AT 00:47Augusta Barlow
December 8, 2025 AT 09:51Joe Lam
December 8, 2025 AT 20:16Jenny Rogers
December 9, 2025 AT 07:02Rachel Bonaparte
December 10, 2025 AT 20:23Chase Brittingham
December 11, 2025 AT 18:22Ollie Newland
December 13, 2025 AT 05:58jagdish kumar
December 15, 2025 AT 01:27michael booth
December 16, 2025 AT 12:06Carolyn Ford
December 17, 2025 AT 13:11