
Diphenhydramine Overdose Risk Calculator
This calculator estimates your risk of diphenhydramine (Benadryl) overdose based on body weight and amount consumed. It is not a substitute for medical advice.
Most people think of diphenhydramine as a harmless sleep aid or allergy pill. It’s in medicine cabinets everywhere-Benadryl, Tylenol PM, Nytol. But taking just a few extra pills can turn a quiet night’s rest into a life-threatening emergency. In 2022, over 14,000 people in the U.S. called poison control because of diphenhydramine overdose. Many were teens chasing a high. Others accidentally took too much while mixing meds. The truth? This isn’t just about drowsiness. It’s about seizures, heart attacks, and brain damage.
What Happens When You Take Too Much Diphenhydramine?
Diphenhydramine blocks acetylcholine, a brain chemical that controls movement, memory, and muscle control. At normal doses, that’s why it makes you sleepy. But when you take too much-usually more than 5 mg per kilogram of body weight-that blockage goes into overdrive. The result? A cluster of symptoms doctors call anticholinergic toxidrome.
Think of it like this: your body’s internal switches get stuck in the "off" position. You get dry as a bone-no saliva, no sweat, no tears. Your skin turns red as a beet and feels hot to the touch. Your pupils become blind as a bat-huge, fixed, unresponsive to light. You can’t see clearly. You can’t urinate. Your heart races. And your mind? It goes haywire. Hallucinations. Paranoia. Confusion so bad you don’t recognize your own family.
At doses over 20 mg per kg (about 1,400 mg for a 70 kg adult), things turn deadly. The drug starts blocking sodium channels in your heart-same way tricyclic antidepressants do. That’s when your EKG shows a widened QRS complex (>100 ms). That’s when your blood pressure drops. That’s when your heart starts beating irregularly. Seizures kick in. Body temperature soars past 40°C. You’re not just overdosing. You’re in cardiac and neurological collapse.
Who’s at Risk?
It’s not just intentional overdoses. Kids under six accidentally swallow pills because they look like candy. Older adults mix diphenhydramine with other meds and don’t realize the danger. But the biggest surge? Teens and young adults.
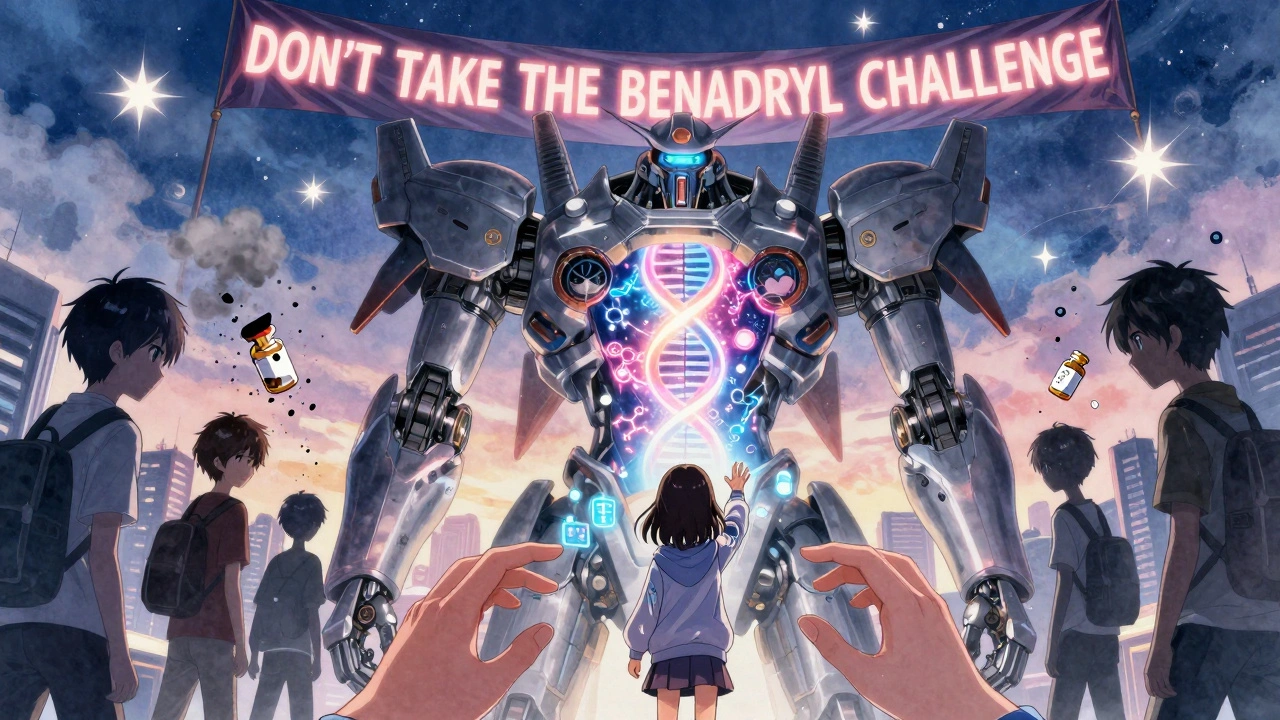
Social media challenges-like the "Benadryl challenge"-have turned this into a dangerous trend. Videos show people swallowing 10, 20, even 30 pills to "get high." One Reddit user posted: "Took 600 mg thinking I’d trip. Woke up in the ER with a catheter. Didn’t remember anything." Between 2018 and 2022, intentional overdoses in teens tripled. Poison control centers report that 43% of cases now involve people under 20.
And it’s not just the pills. Many products combine diphenhydramine with acetaminophen-like Tylenol PM. People think they’re just taking a sleep aid. They don’t realize they’re also risking liver damage. That’s why checking labels matters. That’s why calling poison control immediately is non-negotiable.
What Doctors Look For in the ER
If someone comes in after taking too much diphenhydramine, the ER team doesn’t waste time guessing. They go straight to the ABCDE protocol: Airway, Breathing, Circulation, Disability, Exposure.
First: vital signs. Heart rate over 120? Temperature above 38°C? Blood pressure low? That’s a red flag. Then: the EKG. A widened QRS complex is the most important sign of severe toxicity. QT prolongation? That’s another warning. They’ll check acetaminophen levels-even if the patient says they didn’t take it-because combination products are so common.
They’ll also test creatine phosphokinase (CPK). High levels mean muscle breakdown-rhabdomyolysis-which can lead to kidney failure. Blood tests for electrolytes and kidney function? Standard. But here’s the catch: blood levels of diphenhydramine itself? Not useful. You can’t use them to guide treatment. Symptoms matter more than numbers.
And yes-they’ll check for other drugs. People often mix diphenhydramine with alcohol, opioids, or stimulants. That changes everything.

How It’s Treated
There’s no antidote that just reverses it. Treatment is all about managing symptoms-fast and aggressively.
Seizures or severe agitation? Benzodiazepines-diazepam or lorazepam-are first-line. They calm the brain. No exceptions.
QRS widening over 100 ms? Sodium bicarbonate. A bolus, then an IV drip. It pushes sodium into heart cells and fixes the electrical block. This can be lifesaving.
QTc over 500 ms? Magnesium sulfate. It stabilizes the heart rhythm.
Delirium, hallucinations, confusion? This is where things get interesting. For years, doctors avoided physostigmine because they feared it could trigger seizures or heart problems. But new data from 2021 to 2023 shows it’s safer than we thought. In one study, 87% of patients with severe delirium improved with physostigmine-compared to just 24% with benzodiazepines alone. It crosses the blood-brain barrier and reverses the anticholinergic effects. But it’s not for everyone. If the patient has seizures or a prolonged QRS, you stick with benzodiazepines.
High fever? Cooling blankets, ice packs, IV fluids. Temperatures above 39°C can cause brain damage. Don’t wait.
Can’t urinate? Catheterization. In 35-40% of moderate to severe cases, the bladder is so full it’s distended. It’s painful. It’s dangerous. It needs to be drained.
Cardiac arrest? In rare, extreme cases, doctors have used intravenous lipid emulsion or even ECMO-machine-assisted circulation-to keep patients alive while their bodies recover.
What Happens After?
Even if someone wakes up and seems fine, they’re not out of the woods. Diphenhydramine stays in the system for hours-sometimes days. Symptoms can return 6-12 hours after ingestion.
That’s why observation is critical. The American Association of Poison Control Centers recommends monitoring for at least 4-6 hours after symptoms resolve. If there were cardiac issues? 12-24 hours. Some patients report lingering confusion for 24-48 hours. Others can’t sleep for days. Urinary retention? It can take a week to fully resolve.
And the psychological impact? Real. Teens who took part in the Benadryl challenge often describe lasting anxiety, nightmares, and guilt. One 17-year-old told a counselor: "I thought I was being cool. I didn’t know I could die from a pill I bought at the pharmacy."
How to Prevent It
Education is the best defense. The FDA issued a warning in 2021. The American Academy of Pediatrics launched "Don’t Take the Benadryl Challenge" campaigns on TikTok and Instagram. Poison control centers now promote apps like Poison Help, which has been downloaded over 150,000 times since 2021.
Parents: lock up medications. Even if your child seems responsible, curiosity and peer pressure are powerful. Keep all medicines out of reach-not just in the bathroom cabinet, but in a locked drawer.
Adults: read labels. Check for diphenhydramine in sleep aids, cold meds, and pain relievers. Don’t combine them. Don’t assume "natural" or "over-the-counter" means safe.
If you’re ever unsure-call poison control. In the U.S., it’s 1-800-222-1222. In Australia, it’s 13 11 26. Don’t wait for symptoms. Don’t Google it. Call immediately. Every minute counts.
What Experts Say
Dr. Robert Hendrickson, a medical toxicologist at Oregon Health & Science University, puts it plainly: "Diphenhydramine toxicity is often underestimated because it’s perceived as a benign over-the-counter medication. But its cardiac sodium channel blocking effects can be as dangerous as tricyclic antidepressant overdose in large quantities."
Emergency doctors in Chicago report full recoveries when treatment starts early. But they also see the worst outcomes when people wait too long. "We had a 16-year-old come in with a QRS of 140 ms. He coded on arrival. We got him back. But he had brain damage. He’ll never be the same."
There’s no magic pill. No quick fix. Just one rule: if you suspect an overdose, act fast. The difference between life and death isn’t always the dose. It’s the response time.
Can you die from a diphenhydramine overdose?
Yes. While fatalities are rare-estimated at 0.5% in severe cases-they do happen. Death usually results from cardiac arrest, seizures, or extreme hyperthermia. Doses over 20 mg per kg are considered life-threatening. Early treatment greatly improves survival.
How much diphenhydramine is too much?
For adults, the maximum single dose is 50 mg. Toxic effects start around 5 mg per kg of body weight (about 350 mg for a 70 kg person). Doses over 20 mg per kg (1,400 mg or more) are potentially fatal. Many overdose cases involve 600-1,000 mg taken at once.
Is physostigmine safe for treating diphenhydramine overdose?
Yes, when used correctly. Once considered risky, recent studies show physostigmine is safe and effective for reversing severe anticholinergic delirium. Adverse events occur in under 5% of cases and include mild nausea or temporary QT prolongation. It’s contraindicated only if the patient has seizures or a widened QRS complex on EKG.
Can diphenhydramine cause long-term brain damage?
In severe cases, yes. Prolonged seizures, extreme hyperthermia, or cardiac arrest can lead to hypoxic brain injury. Survivors of massive overdoses sometimes report lasting memory problems, confusion, or difficulty concentrating-even after full physical recovery.
What should I do if someone takes too much Benadryl?
Call poison control immediately-don’t wait for symptoms. In the U.S., dial 1-800-222-1222. In Australia, call 13 11 26. Do not induce vomiting. Keep the person awake and monitor breathing. If they’re confused, having seizures, or turning blue, call emergency services right away. Time is critical.
Why do teens take diphenhydramine to get high?
Social media challenges falsely claim that high doses cause hallucinations or euphoria. Many teens don’t realize the risks. They see videos of people acting strangely after taking 10-20 pills and think it’s safe or cool. The reality is terrifying: confusion, paralysis, heart problems, and sometimes death.

Linda Migdal
December 1, 2025 AT 17:29Diphenhydramine isn't a "sleep aid"-it's a chemical weapon disguised as a pharmacy staple. The FDA's warning? Too little, too late. We're letting Big Pharma turn OTC meds into recreational ammo. This isn't about "bad choices"-it's about systemic negligence. Every pharmacy shelf should have a warning label that screams "THIS CAN KILL YOU IN 45 MINUTES." And no, "read the label" isn't enough when the label's printed in 6-point font next to a cartoon bunny.
Tommy Walton
December 1, 2025 AT 18:49Existential question: if a pill makes you hallucinate but you don’t remember it… did it even happen? 🤔 We’re all just meat puppets dancing to neurotransmitter strings. Diphenhydramine doesn’t kill-it reveals. The veil is thin, my friends. And the FDA? They’re just priests of the placebo temple. 🕊️
soorya Raju
December 2, 2025 AT 15:24u think this is about benadryl? nah. this is a psyop. the gov wants us to think otc meds are dangerous so we’ll start taking their "approved" brain drugs. also, the 14,000 overdose cases? fake. they counted every kid who took 2 pills and sneezed. and why is physostigmine "safe" now? because they found a way to patent it. they been hiding this cure for 30 years. #cointelpro #benadrylisabillgatesproject
Grant Hurley
December 4, 2025 AT 05:15man i used to take 4 benadryl to chill out back in college. never thought twice. now i see those videos of kids doing 600mg and i just wanna hug them and say "bro, you're not tripping-you're one step away from not waking up." glad this post exists. we need more real talk like this. no judgment, just care. 🙏
Nnaemeka Kingsley
December 6, 2025 AT 00:14in my country we use this medicine for cough and cold. never knew it can kill. thank you for sharing. my cousin take 10 pills once because he thought it make him sleep better. he was in hospital 3 days. now he say he never touch again. please tell more people. safety first.
Kshitij Shah
December 7, 2025 AT 14:45oh wow, so now we're treating anticholinergic toxidrome like it's a TikTok trend? next they'll be selling "Benadryl High Starter Pack" with a free catheter and a QR code to poison control. classic. 🙃
Sean McCarthy
December 8, 2025 AT 10:08Let me be clear. This is not a "challenge." It is not "edgy." It is not "cool." It is a medical emergency. Every single person who participates in this is either dangerously ignorant or actively suicidal. There is no middle ground. No nuance. No justification. Stop romanticizing it. Stop normalizing it. Stop. It. Now.
Jaswinder Singh
December 10, 2025 AT 05:08bro this is why we need to stop acting like OTC means "safe." my uncle died from mixing this with his blood pressure med-he didn’t even know it was in there. you think the pharmacy cares? nah. they just want you to buy more. this isn’t about teens being dumb-it’s about corporations not giving a fuck. wake up.
Bee Floyd
December 10, 2025 AT 08:26For anyone reading this and thinking "I’d never do that"-you’re probably right. But maybe you know someone who does. Maybe they’re scrolling right now, wondering if it’s worth it. Don’t just scroll past. Send them this. Say something. Even just "hey, I care." It might be the only thing that stops them.
Jeremy Butler
December 11, 2025 AT 05:56It is imperative to underscore that the pharmacological profile of diphenhydramine, particularly its anticholinergic activity, constitutes a significant neurophysiological perturbation. The potential for irreversible cerebral hypoxia, coupled with the delayed onset of cardiac arrhythmias, demands a paradigmatic shift in public health messaging. The current regulatory framework is insufficiently robust to mitigate emergent behavioral epidemiologies. A mandatory, standardized, and linguistically unambiguous warning system must be instituted across all pharmaceutical packaging, commensurate with the severity of the risk. The normalization of recreational pharmacology in digital culture is not merely a social phenomenon-it is a public health catastrophe in slow motion.