Every year, millions of people reach for an OTC medication before calling a doctor. It’s common. It’s convenient. But many don’t realize that just because a drug is sold over the counter doesn’t mean it’s harmless. OTC medications are powerful tools - and like any tool, using them wrong can cause real harm.
What Are OTC Medications, Really?
OTC medications are drugs you can buy without a prescription. They’re meant for short-term relief of mild, self-diagnosable issues like headaches, colds, heartburn, or allergies. In the U.S. alone, there are more than 800 active ingredients in over 100,000 different products. That’s not just aspirin and cough syrup - it’s everything from nasal sprays to antacids to anti-dandruff shampoos. The FDA and similar agencies worldwide regulate these to ensure they’re safe when used as directed.
But here’s the catch: 25% of adults believe OTC means “always safe,” no matter how much you take. That’s dangerously wrong. In fact, 68% of accidental overdoses involve OTC drugs. You don’t need a doctor’s note to buy them - but you do need to understand what you’re taking.
Pain Relievers: Acetaminophen vs. NSAIDs
If you have a headache or fever, chances are you grab acetaminophen (Tylenol) or an NSAID like ibuprofen (Advil) or naproxen (Aleve). Both work, but they work very differently.
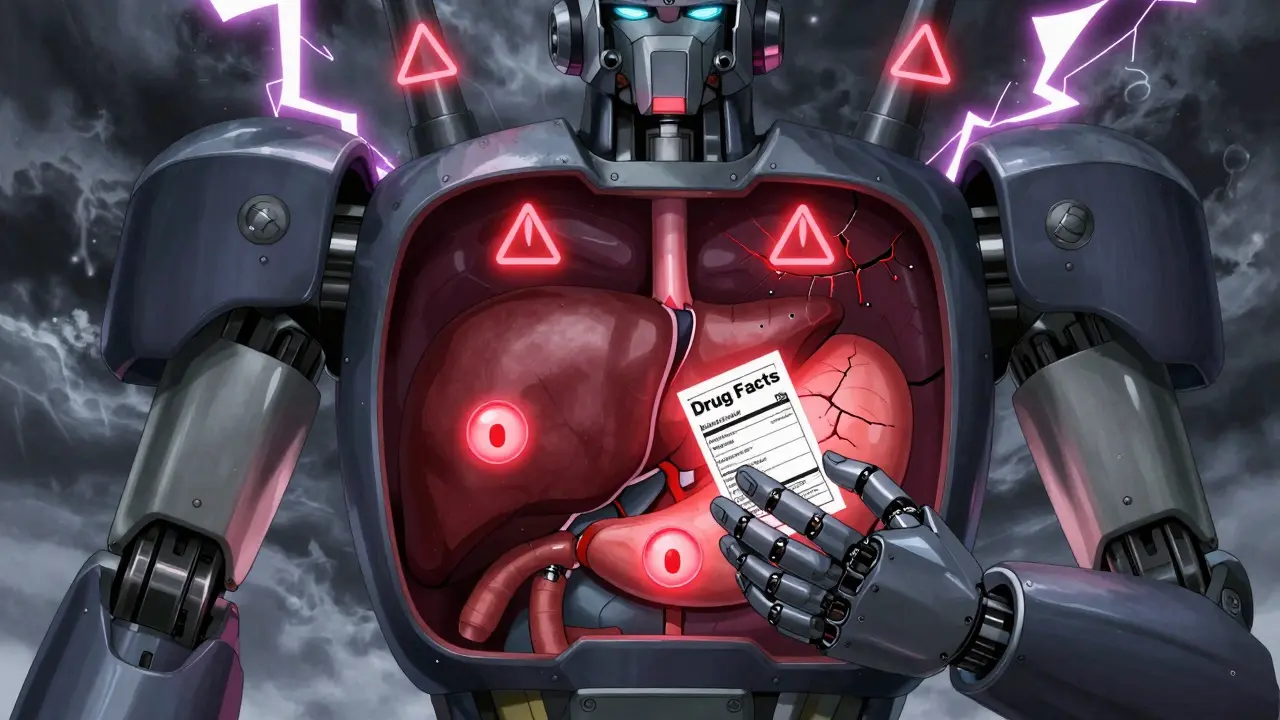
- Acetaminophen reduces pain and fever but doesn’t fight inflammation. It’s often preferred for kids, pregnant people, or those with stomach issues. But it’s hard on the liver. The maximum daily dose is 4,000 mg - and many people hit that without realizing it. Cold medicines, pain relievers, and even some sleep aids contain acetaminophen. Taking two products with it? That’s how liver damage happens. The FDA reports 15,000-18,000 emergency cases each year from acetaminophen overdose.
- NSAIDs like ibuprofen (200-800 mg per dose) and naproxen (220 mg per tablet) reduce inflammation, swelling, and pain. Great for sprains, arthritis, or menstrual cramps. But they irritate the stomach lining. Long-term use can lead to ulcers or internal bleeding. People with kidney disease, high blood pressure, or a history of stomach ulcers should avoid them. And if you’re over 65, talk to a pharmacist before using them regularly.
Bottom line: Don’t assume one is “better.” Use acetaminophen for fever or mild pain. Use NSAIDs for swelling or muscle pain. Never mix them unless your doctor says so.
Cold, Flu, and Allergy Meds: What’s in Your Bottle?
When you have a runny nose or itchy eyes, you might grab a multi-symptom cold tablet. But here’s the problem: those pills often contain four or five different drugs - and you probably don’t need all of them.
- Pseudoephedrine (Sudafed) helps with nasal congestion. It’s effective, but it can raise blood pressure. Some stores keep it behind the counter because it’s used to make illegal drugs. You need to show ID to buy it.
- Dextromethorphan (Delsym) suppresses coughs. Sounds harmless, right? But teens are abusing it for its hallucinogenic effects. The FDA has seen a rise in ER visits from overdoses.
- Guaifenesin (Mucinex) thins mucus. It helps if you’re coughing up phlegm. But it won’t stop a dry cough.
- Diphenhydramine (Benadryl) is an old-school antihistamine. It works - but it makes you drowsy. Avoid it if you drive, operate machinery, or are over 65. Studies show it increases fall risk by 30% in older adults.
- Loratadine (Claritin) and fexofenadine (Allegra) are newer antihistamines. They work just as well, with 90% less drowsiness. If you have allergies, these are smarter choices.
Pro tip: Skip combination products unless you have all the symptoms. Taking a “full-spectrum” cold medicine when you only have a runny nose means you’re getting unnecessary drugs - and side effects - for no reason.
Heartburn and Digestive Aids: More Than Just Tums
Heartburn is common. So are OTC remedies. But not all are equal.
- Antacids like Tums (calcium carbonate) give quick relief by neutralizing acid. They’re fine for occasional use. But if you take them daily, you might get constipation or high calcium levels.
- H2 blockers like famotidine (Pepcid AC) reduce acid production. They work slower than antacids but last longer. Safe for most people.
- Proton pump inhibitors (PPIs) like omeprazole (Prilosec OTC) are the strongest. They’re great for frequent heartburn - but not for daily, long-term use. A 2023 JAMA study found that using PPIs for more than a year increases the risk of chronic kidney disease by 20-50%. Don’t use them for months on end without seeing a doctor.
Also, watch out for hidden sugars. Some liquid antacids and chewables contain sugar or artificial sweeteners. If you have diabetes, check the label.
Special Populations: Kids, Seniors, and Pregnant People
OTC meds aren’t one-size-fits-all. Certain groups need extra caution.
- Children under 4: The FDA banned cough and cold medicines for this age group after 115 deaths between 1969 and 2006. Even small doses can cause seizures or breathing problems. Use saline drops and a humidifier instead.
- Pregnant people: Acetaminophen is the only recommended pain reliever during pregnancy. NSAIDs like ibuprofen can harm fetal kidneys after week 20. Avoid them completely in the third trimester.
- Adults over 65: Your body processes drugs slower. Diphenhydramine (Benadryl) increases fall risk. NSAIDs can trigger kidney issues. Even low-dose aspirin can cause bleeding. Always ask your pharmacist before starting anything new.

How to Use OTC Meds Safely
Here’s how to avoid common mistakes:
- Read the Drug Facts label: Since 2023, all OTC products in the U.S. must use a standardized label. Look for: active ingredient, purpose, uses, warnings, and directions. If you can’t find it, don’t take it.
- Check for duplicates: Many cold, flu, and allergy meds contain the same active ingredients. Taking two at once = overdose risk.
- Don’t use them long-term: OTC meds are for short-term relief. If your symptoms last more than 7-10 days, see a doctor. Using OTC painkillers for chronic back pain? That’s not what they’re for.
- Store them properly: Keep them in a cool, dry place. Heat and humidity ruin potency. Most expire in 2-3 years. Don’t use expired meds.
- Talk to your pharmacist: Pharmacists are trained to catch dangerous interactions. If you take blood pressure meds, diabetes drugs, or antidepressants, ask if your OTC choice is safe. 93% of Americans live within 5 miles of a pharmacy. Use that resource.
The Bigger Picture: OTC Medications and Public Health
OTC drugs saved billions in healthcare costs. They let people manage minor issues without crowding ERs. But misuse is rising. In 2023, the National Institute on Drug Abuse reported 1.2 million emergency visits tied to OTC meds - mostly from dextromethorphan abuse and accidental overdoses.
Companies are trying to fix this. CVS Health launched an AI app that checks your meds and warns about risks. Pharmacists are being trained to give mandatory counseling on high-risk products. And regulators are tightening rules - the European Medicines Agency now requires 10+ years of safety data before approving an OTC drug.
The future isn’t about more OTC drugs. It’s about smarter use. Knowing when to take them - and when to walk away - is the real skill.
Can I take OTC pain relievers every day?
No. OTC pain relievers like acetaminophen and ibuprofen are meant for short-term use - usually no more than 10 days for pain or 3 days for fever. Daily use increases the risk of liver damage (acetaminophen), stomach bleeding (NSAIDs), and kidney problems. If you need daily pain relief, see a doctor. There may be an underlying condition that needs treatment.
Is it safe to take OTC meds while pregnant?
Acetaminophen is considered the safest pain reliever during pregnancy. Avoid NSAIDs like ibuprofen and naproxen, especially after 20 weeks, as they can affect fetal kidney development. For allergies, loratadine (Claritin) and fexofenadine (Allegra) are preferred over diphenhydramine (Benadryl). Always check with your OB-GYN before taking anything, even if it’s labeled “OTC.”
Why are some OTC drugs kept behind the counter?
Some OTC drugs, like pseudoephedrine (found in Sudafed), are kept behind the counter because they can be used to make illegal drugs like methamphetamine. The U.S. government requires pharmacies to log purchases and limit how much you can buy at once. You also need to show ID. This doesn’t mean they’re prescription-only - just that they’re regulated more strictly.
Can OTC meds interact with my prescription drugs?
Yes, and this is one of the most dangerous risks. For example, NSAIDs can raise blood pressure and reduce the effectiveness of blood pressure meds. Acetaminophen can increase bleeding risk if you take blood thinners like warfarin. Even common supplements like St. John’s Wort can interfere with antidepressants. Always tell your pharmacist about every prescription, supplement, and OTC drug you take - even if you think it’s unrelated.
What should I do if I think I’ve overdosed on an OTC drug?
Call emergency services or Poison Control immediately. Don’t wait for symptoms. Acetaminophen overdose can cause liver failure without noticeable signs for hours. For NSAIDs, symptoms like vomiting, dizziness, or confusion can signal serious toxicity. Keep the medication bottle handy - it helps medical staff identify the active ingredient and dose.
Are natural remedies safer than OTC meds?
Not necessarily. Many herbal supplements aren’t regulated like OTC drugs. They can have unpredictable doses, contaminants, or dangerous interactions. For example, willow bark acts like aspirin and can cause bleeding. Licorice root can raise blood pressure. Just because something is “natural” doesn’t mean it’s safe. Always treat herbal remedies like medicine - research them and talk to a pharmacist.
Final Thoughts: OTC Doesn’t Mean Risk-Free
OTC medications are a huge part of modern healthcare. They’re affordable, accessible, and effective - when used correctly. But they’re not candy. Every pill has consequences. The best way to stay safe? Know what’s in your medicine cabinet. Read the label. Ask questions. And if something doesn’t feel right - stop and call a professional.

Antwonette Robinson
February 4, 2026 AT 14:56Oh honey, you mean that ‘OTC’ doesn’t stand for ‘Oh That’s Completely Safe’? 🤦♀️ I thought it was like buying candy. Turns out, my ‘quick fix’ for my headache was slowly murdering my liver. Thanks for the wake-up call, I guess.
Prajwal Manjunath Shanthappa
February 4, 2026 AT 23:35Let me just say-this article, while technically accurate, is so fundamentally naive as to be almost offensive. The FDA? Please. They’re a regulatory arm of Big Pharma’s marketing division. The real danger isn’t acetaminophen-it’s the systemic collapse of medical literacy. You don’t need to ‘read the label’-you need to understand pharmacokinetics. I’ve seen patients self-administer 12,000 mg of APAP over three days… and then wonder why their ALT is 1800. Pathetic.
And don’t get me started on ‘natural remedies.’ Willow bark? That’s salicin. Aspirin. Without the safety data. Without the dosing guidelines. Without the accountability. You’re not ‘being holistic’-you’re playing Russian roulette with your hepatocytes.
rahulkumar maurya
February 5, 2026 AT 18:03Most people don’t even know what ‘active ingredient’ means. They see ‘Tylenol Cold + Flu’ and think it’s a magic potion. Meanwhile, they’re stacking it with Excedrin, NyQuil, and that ‘herbal energy booster’ from the gas station. It’s like driving a car with five gas pedals and no brakes. And you wonder why ERs are full? It’s not the system-it’s the people. The system works fine if you don’t treat it like a buffet.
Also, ‘consult your pharmacist’? Ha. Most pharmacists are overworked, underpaid, and on their third coffee. They’ll nod and say ‘yes’ while you’re already halfway to liver failure. Knowledge is power. But most people don’t even know what power means.
pradnya paramita
February 6, 2026 AT 07:58Key point missed: the CYP450 enzyme system. Acetaminophen is metabolized via CYP2E1, and ethanol induction significantly increases NAPQI formation-leading to hepatotoxicity. NSAIDs inhibit COX-1, reducing gastric mucosal protection. PPIs suppress acid long-term → hypochlorhydria → bacterial overgrowth → B12 deficiency, malabsorption, and increased C. diff risk. This isn’t just ‘read the label’-it’s understanding metabolic pathways. If you’re on SSRIs, watch for serotonin syndrome with dextromethorphan. It’s not folklore-it’s pharmacology.
Also: loratadine’s half-life is 8–12 hours. Fexofenadine’s is 11–15. Diphenhydramine? 3–8 hours, but anticholinergic burden accumulates. In elderly, that’s dementia risk. Not ‘drowsiness.’ Neurotoxicity.
Ed Mackey
February 6, 2026 AT 14:56Hey, I just wanted to say thanks for this. I’ve been taking ibuprofen every day for my back for like 2 years. I didn’t realize it could mess with my kidneys. I’m gonna go see my doc this week. Also-my grandma used to say ‘if it’s on the shelf, it’s not a big deal.’ Guess she was wrong. 🙃
Also, I think I accidentally took two cold meds once. Felt weird for a few hours. Didn’t think to check the ingredients. Rookie mistake.
Jhoantan Moreira
February 8, 2026 AT 14:38This is such a needed conversation 💙 Honestly, I didn’t know about the kidney risk with PPIs. My mom’s been on omeprazole for 5 years. I’m gonna talk to her tonight. Also, I love that you mentioned pharmacists-they’re the unsung heroes of public health. Next time I’m at the store, I’m gonna say hi to mine and ask if my supplements are safe. Small acts, right? 😊
Alex LaVey
February 10, 2026 AT 08:28As someone who grew up in a family that treated medicine like a grocery list, I can’t tell you how much I appreciate this. My dad used to take 4 Advil and 2 Tylenol at once ‘because he felt worse.’ We thought it was normal. Now I’m the one teaching my nieces to read labels. It’s not about fear-it’s about empowerment. Keep spreading this. We need more of it.
caroline hernandez
February 11, 2026 AT 06:47Let’s talk about the antihistamine trap. Diphenhydramine is the OG, but it’s also the OG of anticholinergic burden. In geriatric patients, it’s linked to cognitive decline, urinary retention, constipation, and delirium. Loratadine? Clean. Fexofenadine? Cleaner. And don’t even get me started on OTC sleep aids that are just Benadryl in disguise. You’re not ‘sleeping’-you’re sedating your brain into a fog. That’s not rest. That’s chemical downtime.
Pro tip: If you’re using OTC meds for more than 3 days, you’re not managing-you’re masking. And masking isn’t healing.
Joseph Cooksey
February 12, 2026 AT 12:01Okay, let’s get real. The entire OTC system is a corporate circus. You think they want you to understand CYP450? Nah. They want you to buy three different bottles of ‘Cold & Flu’ because you can’t read. The label? Designed to confuse. The ‘active ingredients’ section? A maze. And the ‘warnings’? Printed in font size 5. Meanwhile, Big Pharma is making billions off the fact that 70% of Americans can’t read past the third grade. It’s not ignorance-it’s design. And don’t even get me started on how they rebrand the same drug under 12 different names. That’s not innovation. That’s exploitation.
And yes, I know someone who took ‘Delsym’ because they heard it ‘helped with anxiety.’ They ended up in the ER with hallucinations. The company? Still selling it. With a smile.
Meenal Khurana
February 14, 2026 AT 03:58Read the label. Always.
Sherman Lee
February 14, 2026 AT 19:10Did you know the FDA allows OTC drugs to be sold without double-blind trials? That’s right. They use ‘historical use’ as evidence. Meanwhile, every time you take a NSAID, you’re rolling dice with your GI tract. And the ‘natural remedies’? They’re not regulated at all. One batch of echinacea has 2% active compound. Next batch? 18%. And no one’s checking. I think this whole system is a controlled experiment. And we’re the lab rats.
Also… who really owns the pharmacy shelves? 🤔
Amit Jain
February 15, 2026 AT 03:33I work in a pharmacy in Mumbai. Every day, someone comes in with 5 different OTC pills. They say, ‘I just need something for fever.’ I ask, ‘What’s in the other bottles?’ They don’t know. I explain. They leave. Next day, they come back with the same problem. It’s not about knowledge-it’s about habit. I just keep trying. One person at a time.
Antwonette Robinson
February 16, 2026 AT 15:05Wow. Someone actually read the label. Who even are you? 🤨