For years, doctors told people with cirrhosis to cut back on protein. The idea was simple: less protein means less ammonia, and less ammonia means fewer episodes of confusion or brain fog from hepatic encephalopathy. But that advice was wrong. And sticking to it could be killing you.
Why Protein Isn’t the Enemy in Cirrhosis
Cirrhosis isn’t just a damaged liver-it’s a body-wide metabolic crisis. Your liver can’t process nutrients the way it used to, and your muscles start breaking down just to keep you alive. This isn’t normal aging. This is your body eating itself, slowly, day by day. And the main fuel for that self-destruction? Your own muscle tissue. In the 1990s, it was common to restrict protein to 40-60 grams a day for people with cirrhosis. That’s less than a single chicken breast. But a landmark study in 2004 changed everything. Researchers gave one group of patients only 0.5 grams of protein per kilogram of body weight, and another group 1.2 grams. The low-protein group didn’t get fewer episodes of brain fog. Instead, they lost muscle faster-and their bodies started breaking down even more tissue to survive. The higher-protein group? They stayed stronger. Their ammonia levels didn’t spike. Their survival rates improved. Today, every major liver association-AASLD, EASL, the British Liver Trust-agrees: protein restriction is harmful. It doesn’t protect your brain. It destroys your body.How Much Protein Do You Really Need?
You don’t need to eat like a bodybuilder. But you do need to eat enough to stop the muscle loss. For most people with stable cirrhosis, aim for 1.2 to 1.5 grams of protein per kilogram of dry body weight. That’s your weight without the extra fluid swelling in your belly or legs. If you weigh 70 kg (about 154 lbs) and have fluid retention, your dry weight might be 60 kg. That means 72-90 grams of protein a day. If you’re already losing muscle-sarcopenia is present in 40-70% of cirrhosis patients-you should push toward 1.5 grams per kg. If you’re hospitalized or very ill, you may need up to 2.0 grams per kg. Here’s a simple way to estimate it: if you weigh 150 pounds, that’s about 68 kg. Aim for 80-100 grams of protein daily. That’s not a lot when you break it down:- 2 large eggs = 12 grams
- 1 cup Greek yogurt = 18 grams
- 3 oz chicken breast = 27 grams
- 1 cup lentils = 18 grams
- 1 cup milk = 8 grams
Where to Get Your Protein (And What to Avoid)
Not all protein is created equal in cirrhosis. Meat-based proteins-beef, pork, chicken, fish-are high in protein, but they’re harder for some people to tolerate. That’s because they contain more aromatic amino acids, which can trigger brain fog in sensitive individuals. The better options? Plant and dairy sources.- Beans, lentils, chickpeas
- Tofu, tempeh, edamame
- Low-sodium cheese, cottage cheese
- Yogurt (unsweetened, plain)
- Eggs
- Nuts and seeds (almonds, pumpkin seeds)
- Oatmeal, quinoa, soy milk
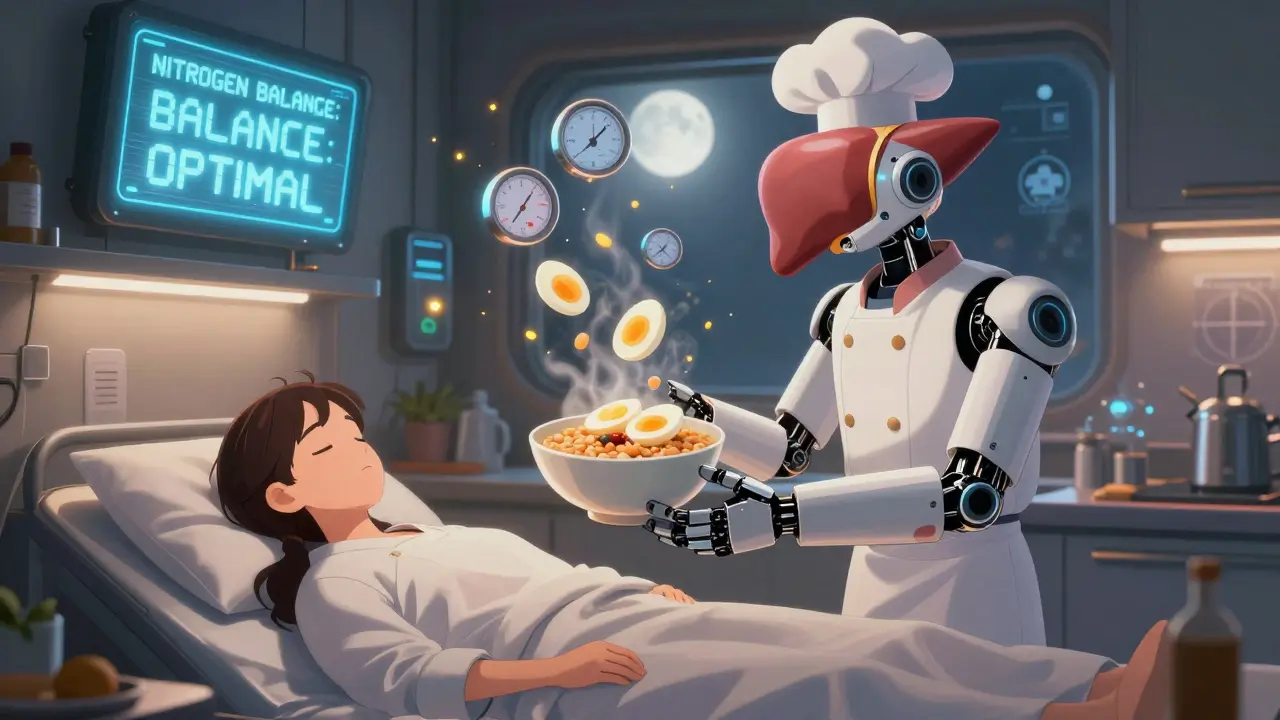
Timing Matters More Than You Think
It’s not just how much protein you eat-it’s when. Cirrhosis turns your body into a muscle-burning furnace overnight. If you go 8-10 hours without eating, your body starts breaking down muscle to make energy. That’s why skipping dinner or fasting is dangerous. Experts recommend eating every 3-4 hours while you’re awake. That means 4-5 small meals a day, not 2 big ones. And you need a protein-rich snack right before bed. A late-night snack isn’t a luxury-it’s medical treatment. Aim for 15-20 grams of protein 1-2 hours before sleep. Examples:- 1 cup cottage cheese with a few almonds
- 2 hard-boiled eggs
- 1 scoop whey protein in water or milk (if tolerated)
- 1 small bowl of lentil soup
Calories Are Just as Important as Protein
You can’t preserve muscle if you’re not getting enough energy. Protein needs to be paired with enough calories. If your BMI is normal, aim for at least 35 kcal per kilogram of dry weight per day. If you’re overweight, adjust downward: 25-35 kcal/kg for BMI 30-40, and 20-25 kcal/kg for BMI over 40. But here’s the catch: many people with cirrhosis feel full fast because of fluid in the belly. So you need calorie-dense foods.- Whole milk instead of skim
- Avocado on toast
- Nut butter on crackers
- Dried fruit like dates or raisins
- Olives, olive oil drizzled on meals
Sodium, Fluids, and the Tough Trade-Off
Many people with cirrhosis are told to cut salt to reduce swelling. But if you’re struggling to eat enough, being too strict with sodium can backfire. The AASLD says: if you can’t meet your protein or calorie goals because of a low-salt diet, it’s okay to relax sodium restrictions a little. Your survival matters more than a few extra millimeters of belly swelling. Work with your doctor or dietitian to find the balance. Maybe you keep salt out of cooking but allow a small amount in protein-rich snacks. Maybe you eat higher-sodium cheese if it helps you eat more. Don’t let sodium rules starve you.Supplements and Micronutrients You Can’t Ignore
Protein and calories aren’t the whole story. Cirrhosis causes hidden deficiencies that wreck your muscles too.- Zinc: Often low. Supplementing 50 mg/day can improve taste, appetite, and even brain function.
- Thiamine (B1): Critical for energy. Many people with cirrhosis are deficient, especially if they’ve had alcohol-related liver disease.
- Magnesium, Folate, B6: Commonly low. These help your body use protein properly.
The Real Cost of Ignoring Protein
This isn’t about feeling stronger. It’s about staying alive. A 2019 study found that people with cirrhosis who had muscle loss were nearly three times more likely to die than those who kept their muscle. That’s not a small risk. That’s the difference between living another year and not. Muscle isn’t just for lifting things. It’s your body’s emergency fuel tank. When your liver fails, your muscles step in. If they’re gone, you have nothing left. The shift in medical thinking is real. What was once considered safe advice-cutting protein-is now recognized as dangerous. And yet, many patients still hear the old warnings. Your doctor might still say “eat less meat.” Your aunt might still tell you “protein is bad for your liver.” Don’t believe them.What to Do Today
Start small. You don’t need to overhaul your diet overnight.- Calculate your dry weight (ask your doctor or dietitian).
- Write down what you ate yesterday. How many grams of protein? If it’s under 1.2 g/kg, you’re falling short.
- Add one protein-rich snack today. Try yogurt or a boiled egg.
- Plan a bedtime snack. Even 10 grams of protein helps.
- Ask your doctor for a referral to a dietitian who specializes in liver disease.
FAQ
Should I avoid protein if I have hepatic encephalopathy?
No. Avoiding protein makes hepatic encephalopathy worse over time by accelerating muscle loss. Multiple studies since 2004 have shown that normal or even high protein intake does not trigger or worsen brain fog in most people with cirrhosis. In fact, protein restriction increases the risk of death. Focus on plant and dairy proteins like beans, tofu, eggs, and yogurt-they’re better tolerated and help preserve muscle.
How do I know if I’m losing muscle?
Signs include feeling weaker when climbing stairs, needing help with daily tasks like standing from a chair, clothes fitting looser around the arms and legs despite weight gain from fluid, or a noticeable thinning of your calves. A simple test: measure your calf circumference. If it’s less than 31 cm for men or 30 cm for women, you likely have muscle loss. Talk to your doctor about a body composition scan or handgrip strength test.
Can I get enough protein without eating meat?
Absolutely. Plant and dairy proteins are often better for people with cirrhosis. A cup of cooked lentils has 18 grams, a cup of Greek yogurt has 18-20 grams, 2 eggs have 12 grams, and tofu provides 10-20 grams per 100 grams. Combine these with nuts, seeds, and soy milk, and you can easily hit your daily target without meat. Many patients report better digestion and fewer brain fog episodes on this approach.
Why is a bedtime snack so important?
Your body goes into muscle-burning mode during overnight fasting. Without food for 8-10 hours, your liver can’t supply glucose, so your muscles break down to make energy. A high-protein snack before bed stops this process, improves nitrogen balance, and helps you wake up stronger. Studies show this single habit reduces muscle loss and improves survival rates.
What if I can’t eat enough food?
Many people with cirrhosis feel full quickly due to fluid in the belly. In that case, focus on calorie- and protein-dense foods: whole milk, nut butter, cheese, dried fruit, olive oil, and avocados. If you still can’t meet targets, ask your doctor about prescription oral nutritional supplements. These are liquid or bar formulas packed with protein, calories, and essential nutrients. They’re not a replacement for food-but they can be lifesaving when eating is hard.

Marc Bains
January 30, 2026 AT 12:25Just got back from my hepatologist and they finally got on board with the protein thing. I was told to cut back for years. My muscles were wasting away. Now I’m eating eggs, Greek yogurt, and lentils daily. I can actually climb stairs without stopping. This isn’t just advice-it’s survival.
Stop listening to outdated doctors. Your muscle is your lifeline.
kate jones
January 31, 2026 AT 10:37Per AASLD 2023 guidelines, plant- and dairy-derived proteins are preferred in hepatic encephalopathy due to their lower aromatic amino acid content, which reduces the risk of triggering neuropsychiatric symptoms. The 1.2–1.5 g/kg dry weight recommendation is evidence-based and aligns with the 2004 seminal study by Mullen et al. Protein restriction remains a class III recommendation-harmful, not beneficial.
Also, don’t neglect zinc and thiamine. Deficiencies here compound sarcopenia and impair protein utilization.
Natasha Plebani
January 31, 2026 AT 22:56It’s ironic, really. We treat cirrhosis like a broken machine that needs to be kept idle-less fuel, less stress. But the body isn’t a car. It’s a living system that adapts, survives, and collapses under neglect. Protein restriction isn’t protective-it’s a surrender.
When your liver fails, your muscle becomes your metabolic reserve. Starving it doesn’t spare the brain-it just hastens the end. We’ve been treating symptoms while ignoring the root: systemic catabolism.
This isn’t nutrition. It’s bioethics. And we’re failing.
Eliana Botelho
February 2, 2026 AT 07:21Okay but what if you’re on a low-sodium diet and you can’t eat cheese or yogurt without bloat? And what if you’re vegan and your gut hates lentils? And what if your doctor says you’re too sick for protein and you’re already in the hospital?
Everyone’s acting like this is one-size-fits-all. It’s not. I’ve seen people die from protein overload because they didn’t have the right enzymes. The real problem? Doctors don’t test for individual tolerance. They just hand out pamphlets.
Also, why is no one talking about gut dysbiosis? That’s where the ammonia really comes from. Fix the gut, not the protein.
Rob Webber
February 2, 2026 AT 22:53Doctors are still pushing this old-school crap because they’re too lazy to read the studies. I’ve had three hepatologists tell me to eat less protein. One even said, ‘Your liver can’t handle it.’ I looked up the 2004 study myself. It proved the opposite.
Stop letting outdated medicine kill you. If your doctor doesn’t know about the AASLD guidelines, find a new one. Your life isn’t a guesswork experiment.
Lisa McCluskey
February 3, 2026 AT 11:37Bedtime snack changed everything for me. Just two eggs before bed. No more waking up weak. My calves stopped shrinking. Simple. Free. Effective.
Also, if you’re struggling to eat, try blending cottage cheese with a banana and almond butter. It’s like a milkshake but packed with protein. No one talks about that.
owori patrick
February 3, 2026 AT 20:53In Nigeria, we use beans, groundnuts, and smoked fish for protein. My uncle with cirrhosis eats pounded yam with peanut soup every day. He’s 72 and still walks to market. No supplements. No fancy diet. Just consistent, traditional food.
Maybe the answer isn’t new science-it’s remembering what worked before the pills and pamphlets came.
Claire Wiltshire
February 5, 2026 AT 10:13Thank you for this comprehensive and compassionate overview. As a dietitian specializing in liver disease, I see daily how protein restriction leads to sarcopenia, increased infection risk, and reduced transplant eligibility. The data is unequivocal.
I encourage all patients to request a referral to a registered dietitian-preferably one with a CNSC or CSSD credential. Personalized plans, including calorie density strategies and supplement options, can make all the difference.
And yes-your bedtime snack matters. It’s not a suggestion. It’s a clinical intervention.
Darren Gormley
February 5, 2026 AT 23:39😂😂😂 so now we’re supposed to eat tofu and yogurt to avoid dying? What’s next? Drinking kombucha for liver detox?
Let me guess-the pharma companies pushed this. Protein powders = big profits. Meanwhile, the real cause? Toxins from processed food and alcohol. Nobody wants to say that.
Also, why are we ignoring the fact that 80% of cirrhosis cases are alcohol-related? Just eat more lentils and call it a day? 😂
Mike Rose
February 6, 2026 AT 05:09bro i just read this and i think the whole protein thing is kinda overhyped
my uncle had cirrhosis and he ate like 2 steaks a day and still died. so maybe it dont matter?
also i think doctors just wanna sell you protein bars. i mean come on.
Russ Kelemen
February 7, 2026 AT 09:50This isn’t just about protein. It’s about reclaiming agency over your body when the system keeps telling you to give up.
Every gram of protein you eat is an act of resistance. Against outdated guidelines. Against fear. Against the idea that you’re too broken to heal.
I’ve watched people go from bed-bound to walking again-not because of a miracle, but because they started eating like their life depended on it. Because it did.
You don’t need perfection. You need persistence. One egg. One yogurt. One bedtime snack. Keep showing up.
Your body remembers every effort. Even when you don’t feel it yet.
Diksha Srivastava
February 8, 2026 AT 18:58I’m from India and my mom has cirrhosis. We started giving her dal, paneer, and boiled eggs every day. She was so weak before-now she laughs again. I cried when she cooked her own meal for the first time in months.
It’s not about fancy science. It’s about love. Feeding someone with care, not fear.
You’re not just eating protein. You’re eating hope.
Yanaton Whittaker
February 10, 2026 AT 01:58Look, I’m proud to be American and we don’t let foreign diet trends kill our people. This protein stuff sounds like some European fad. We’ve been doing it right for decades-low protein, low sodium, no nonsense.
My cousin had cirrhosis and he lived 12 years on a strict low-protein diet. So don’t tell me this new advice is better. I’ve seen the results.
Stick to the American way. We don’t need your tofu and lentils.
Beth Cooper
February 10, 2026 AT 18:06Did you know that the 2004 study was funded by a protein supplement company? And that AASLD now has ties to Big Nutrition? This is all a scam to sell you bars and shakes.
Real doctors know protein restriction works. The real cause of muscle loss? Vaccines. They mess with your mitochondria. That’s why you feel weak.
Also, your liver doesn’t make ammonia-your 5G router does. Turn it off and eat only raw vegetables. I’ve been cured of everything this way.