
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure it actually does? The answer lies in bioequivalence - a scientific standard that bridges the gap between brand-name drugs and their cheaper copies. It’s not about matching ingredients exactly. It’s about proving that your body absorbs and uses the generic drug in the same way as the original. Without this step, generics wouldn’t be trusted by doctors or patients. And without bioequivalence, the entire system of affordable medicines would collapse.
What Bioequivalence Really Means
Bioequivalence isn’t about whether two pills look the same or have the same inactive ingredients. It’s about what happens inside your body after you take them. The FDA defines it as the absence of a significant difference in how quickly and how much of the active drug enters your bloodstream and reaches its target site. If a generic drug delivers the same amount of medicine at the same rate as the brand-name version, it’s considered bioequivalent - no matter how different the pill looks.
This matters because drugs don’t work unless they get into your blood. A tablet might contain the exact same chemical, but if it dissolves too slowly or too fast, your body won’t get the right dose. That’s why the FDA doesn’t just check the label. They test how your body actually responds.
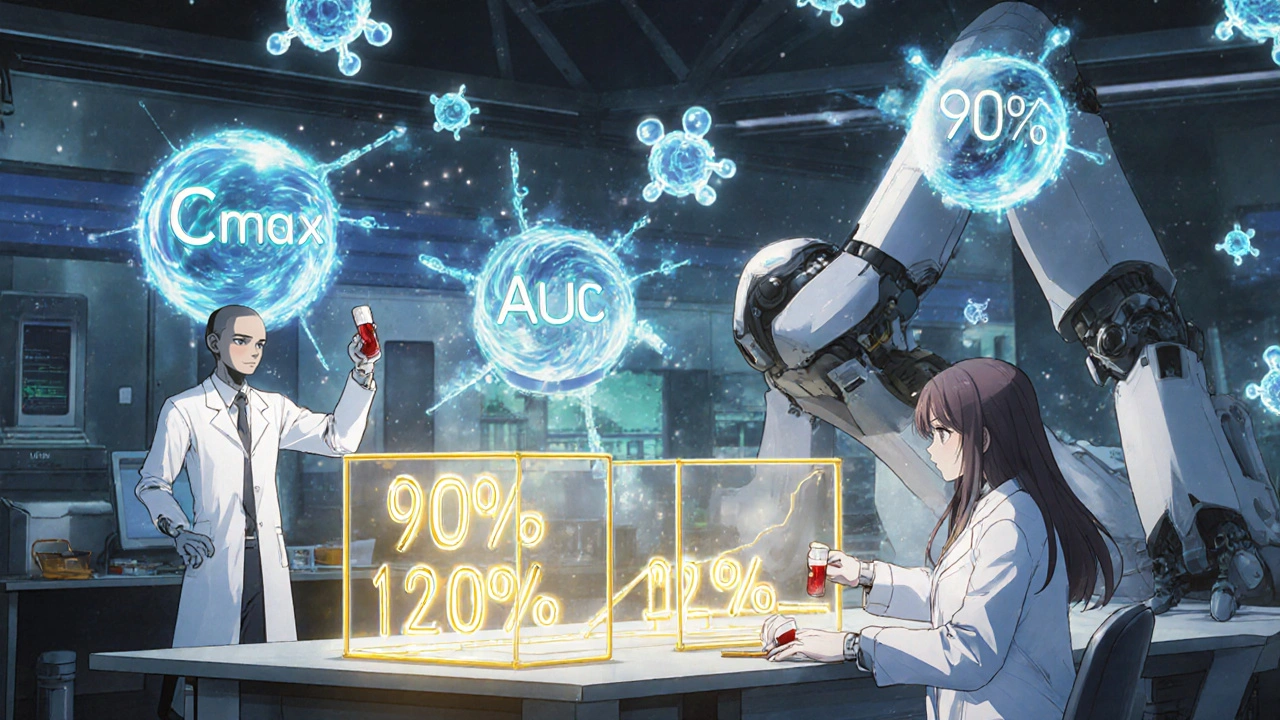
The Two Key Numbers: Cmax and AUC
To measure bioequivalence, scientists run clinical studies with healthy volunteers - usually between 24 and 36 people. Each person takes both the brand-name drug and the generic version, at different times, in a randomized order. Blood samples are taken over hours to track how the drug moves through the body.
Two numbers are critical:
- Cmax: The highest concentration of the drug in the blood. This tells you how fast the drug gets absorbed.
- AUC: The total amount of drug absorbed over time. This tells you how much of the drug your body actually gets.
For a generic to pass, the 90% confidence interval of the ratio between the generic and brand-name drug must fall between 80% and 125% for both Cmax and AUC. That means if the brand-name drug gives you an AUC of 100 units, the generic must deliver between 80 and 125 units. The average result can’t be outside that range, and neither can the full range of possible results.
Here’s a real example: If a generic drug shows an average AUC of 93 (93% of the brand), but the 90% confidence interval runs from 84 to 110, it passes. Even though 93% is below 100%, the entire range fits inside 80-125%. But if the average is 116% and the confidence interval stretches from 103% to 130%, it fails - because 130% is too high.
Common Misconceptions About the 80-125% Rule
Many people think the 80-125% range means a generic drug can contain anywhere from 80% to 125% of the active ingredient. That’s wrong. The rule applies to how your body handles the drug - not how much is in the pill.
The actual amount of active ingredient in a generic must match the brand-name drug exactly. Both must contain the same milligrams of the same chemical compound. The 80-125% range is about absorption - not content. A pill might have 10 mg of the drug, just like the brand. But if it dissolves slowly in your stomach, your body might only absorb 8 mg over time. That’s where bioequivalence testing catches the problem.
The FDA’s standard isn’t a loophole. It’s a safety net. It ensures that even if two pills look different, they behave the same inside your body. And that’s what matters for safety and effectiveness.
Why Not Just Test Patients Instead of Healthy Volunteers?
You might wonder why studies use healthy people instead of patients with the disease. The answer is control. Healthy volunteers don’t have other illnesses, medications, or body changes that could mess with the results. That gives scientists a clean baseline to measure how the drug behaves - without noise.
Once bioequivalence is proven in healthy volunteers, the FDA assumes the same results will hold for patients. That’s because absorption patterns don’t change drastically between healthy and sick people for most drugs. For rare cases where that’s not true - like certain cancer or epilepsy drugs - the FDA may require additional studies. But for the vast majority of medications, the healthy volunteer model is reliable and efficient.
When In Vitro Testing Is Enough
Not all drugs need blood tests. For medications that work locally - like inhalers for asthma, creams for eczema, or eye drops - the drug doesn’t need to enter the bloodstream to work. In those cases, the FDA allows in vitro (lab-based) testing instead.
For example, an inhaler might be tested by measuring how fine the spray is, how much of the drug lands in the lungs, and how quickly it dissolves. If those physical properties match the brand-name product, the FDA accepts that as proof of equivalence. This saves time and avoids unnecessary testing on people.
But for drugs meant to act systemically - like antibiotics, blood pressure pills, or antidepressants - in vivo testing is required. The drug must enter the bloodstream to work, so the FDA needs to see how your body handles it.
What Happens After a Study Fails?
Not every bioequivalence study passes on the first try. In fact, many generics go through multiple rounds of testing before approval. If a study fails, the manufacturer has to figure out why. Maybe the tablet doesn’t dissolve fast enough. Maybe the coating is too thick. Maybe the manufacturing process creates inconsistent颗粒 (particles).
Most failures come down to formulation issues - not the active ingredient itself. That’s why generic companies often work closely with the FDA during development. The agency provides feedback, suggests changes, and even offers guidance documents for over 2,000 specific drugs. These documents tell manufacturers exactly what tests to run, what equipment to use, and what results are acceptable.
Once the formula is fixed, the company runs another study. The process can take months - or even years - for complex drugs. But the FDA doesn’t approve a generic until it’s proven safe and effective.

Transparency and the New Rules
In 2021, the FDA changed its rules to require manufacturers to submit all bioequivalence studies they’ve done - not just the successful ones. Before, companies could hide failed attempts. Now, the FDA sees every test, every result, every outlier.
This change makes the approval process more transparent. It also helps the agency spot patterns. If multiple companies keep failing the same test for a particular drug, the FDA might issue new guidance to help everyone get it right.
This shift reflects a broader trend: regulators are demanding more data, not less. And for patients, that means more confidence in every generic pill they take.
How This Saves Billions
Generic drugs make up about 90% of all prescriptions filled in the U.S., but they cost only about 20% of what brand-name drugs do. Over the last decade, generics saved the healthcare system more than $1.7 trillion. That’s not just a number - it’s millions of people who can afford their medicines because bioequivalence standards keep prices low without sacrificing safety.
The FDA reviews about 1,000 generic applications each year. Bioequivalence studies are the most common reason for delays or rejections. But when a generic passes, it hits the market fast - often within 10 to 12 months. That speed is possible only because the FDA doesn’t make companies repeat every clinical trial ever done for the brand-name drug. They trust the science of bioequivalence.
What’s Next for Bioequivalence?
The FDA is exploring new ways to make bioequivalence testing faster and smarter. One promising area is modeling and simulation. Instead of running full human trials, companies might use computer models to predict how a drug will behave based on its physical properties and past data.
This is already being used for some complex drugs - like topical creams, nasal sprays, and injectables - where traditional testing is hard. If the models prove reliable, they could replace some human studies in the future. That would speed up approvals and lower costs even more.
For now, the 80-125% rule remains the gold standard. It’s simple, proven, and backed by decades of real-world use. Millions of people rely on generics every day. And every single one of those pills passed the same test: bioequivalence.
Do generic drugs have the same active ingredient as brand-name drugs?
Yes. By law, generic drugs must contain the exact same active ingredient, in the same strength and dosage form, as the brand-name drug. The difference isn’t in what’s in the pill - it’s in the inactive ingredients, like fillers or coatings, which don’t affect how the drug works.
Can a generic drug be less effective than the brand-name version?
No - if it’s approved by the FDA. A generic must prove it delivers the same amount of drug into your bloodstream at the same rate as the brand. If it doesn’t meet the 80-125% bioequivalence range, it won’t be approved. Millions of patients use generics safely every day, and clinical outcomes are identical to brand-name drugs.
Why do some people say generics don’t work as well?
Sometimes, people notice differences in size, color, or taste - and assume that means the drug works differently. But those are just inactive ingredients. In rare cases, people may have allergies to fillers in one version. Or, if they’re switching from one generic to another, small differences in absorption can cause temporary side effects. But these aren’t signs of ineffectiveness - they’re variations in formulation, not quality.
Are there drugs where bioequivalence doesn’t apply?
Yes. For drugs that act locally - like inhalers, eye drops, or topical creams - the FDA uses in vitro testing instead of blood tests. For drugs with a very narrow therapeutic index - like warfarin or lithium - doctors may monitor blood levels closely, but the FDA still uses the same 80-125% standard. There’s no evidence that this range fails for these drugs when properly tested.
How long does it take for the FDA to approve a generic drug?
The standard review takes 10 to 12 months. First-cycle approval rates are around 65%, meaning most applications get approved on the first try if they’re well-prepared. Delays usually happen because of incomplete bioequivalence data, formulation issues, or missing documentation. The FDA works with companies to fix problems before rejecting an application.

Eric Healy
November 18, 2025 AT 13:07So let me get this straight - the FDA lets generics be 20% weaker or 25% stronger and calls it ‘equivalent’? That’s not equivalence, that’s a gamble. My aunt took a generic for blood pressure and ended up in the ER. Coincidence? Maybe. But I’m not betting my life on statistics.
Shannon Hale
November 19, 2025 AT 08:25OH MY GOD. I’ve been saying this for YEARS. The 80-125% range is a JOKE. It’s not science, it’s corporate lobbying dressed up in lab coats. You think a pill that absorbs at 82% is the same as one at 124%? That’s like saying a Ferrari and a shopping cart are both ‘vehicles’ so they’re interchangeable. 😤
Holli Yancey
November 19, 2025 AT 11:55I get why the FDA uses healthy volunteers - it’s cleaner data. But I also wonder if we’re missing something by not testing on actual patients. I’ve seen people with chronic conditions react differently to generics, even when they ‘pass’ the tests. Maybe we need more nuance, not just a binary pass/fail.
Gordon Mcdonough
November 19, 2025 AT 13:17Jessica Healey
November 19, 2025 AT 16:39Okay but can we talk about how wild it is that we’re okay with this? We let people take drugs that might absorb differently based on which factory made it. And we call it ‘safe’ because the math is ‘within range.’ Meanwhile, my grandma’s depression meds switch generics every 3 months and she cries for no reason. It’s not her - it’s the pill.
Levi Hobbs
November 21, 2025 AT 12:50I think the FDA’s approach is actually pretty brilliant - it’s not about perfection, it’s about practicality. If you’re delivering 90% of the drug at the right rate, and the variation is statistically controlled, you’re not risking lives - you’re enabling access. Millions of people wouldn’t be able to afford meds without this system. The trade-off is worth it.
henry mariono
November 21, 2025 AT 18:13Just want to say I appreciate the clarity in this post. I used to be skeptical about generics too - until I saw my dad’s diabetes meds switch and his numbers stayed stable. It’s not magic. It’s science. And science doesn’t need drama to be valid.
Sridhar Suvarna
November 22, 2025 AT 00:58Joseph Peel
November 22, 2025 AT 15:26As someone who’s worked in global health, I can tell you this system is why low-income countries can access life-saving meds. The 80-125% rule isn’t a loophole - it’s a lifeline. Without it, we’d be back to rationing insulin and antibiotics. This isn’t just American policy - it’s a global standard for a reason.
Kelsey Robertson
November 24, 2025 AT 00:41Wait - so you’re telling me the FDA approves a drug that could be 25% MORE potent than the brand? And you call that ‘safe’? That’s not bioequivalence, that’s a lottery ticket. What if someone has liver issues? What if they’re elderly? What if they’re on five other meds? You’re not testing for real-world interactions - you’re testing for lab rats in a vacuum. This is dangerous.
Joseph Townsend
November 24, 2025 AT 03:35Y’all are acting like this is the first time someone questioned generics. Let me tell you - back in the 90s, people were throwing tantrums over generic Prozac. ‘It doesn’t work!’ they screamed. Then came the data. Then came the millions of patients who got better. Same with Lipitor. Same with Zoloft. The panic always fades. The science always wins. You’re not special because you’re suspicious - you’re just late to the party.
saurabh lamba
November 26, 2025 AT 00:44bro why are we even talking about this. i took generic metformin for 5 years. no issues. my bank account happy. my sugar stable. end of story. 🤷♂️
Kiran Mandavkar
November 27, 2025 AT 15:37You call this science? This is a grotesque parody of pharmacology - a mathematical sleight-of-hand to justify profit-driven mediocrity. The 80-125% range is not a threshold - it’s a canyon. And we’re all standing on a rope bridge made of placebo psychology and corporate contracts. The FDA doesn’t protect patients - it protects the illusion of affordability. Wake up. The pill you swallow is not your medicine - it’s a compromise.